The Future of AI in Healthcare: 3 Trends to Watch for Moving Into 2026

Oussama Bettaieb
Marketing Director

Share to AI
Ask AI to summarize and analyze this article. Click any AI platform below to open with a pre-filled prompt.
By 2030, we’ll be short 11 million health workers. Hospitals are short-staffed, overbooked, and barely keeping up.
Artificial intelligence in healthcare market has the potential to step in and help. While the technology is rapidly changing how care is delivered, some teams are seeing real results. Others are stuck in pilots that don’t prove ROI.
At Aloa, we help healthcare providers bridge that gap. We build AI that integrates with your systems, protects patient data, and delivers value in care and performance.
Here’s what we’ll cover:
- Where the future of AI in healthcare is heading
- Three major shifts shaping 2026
- How healthcare teams can adopt AI safely and show results that last
Let’s look at what pushed healthcare to this point.
TL;DR
- By 2026, AI will power over 70% of hospital operations, driving efficiency and accuracy.
- AI diagnostics now rival human accuracy (≈0.90 AUC) in imaging, cutting turnaround times by double digits.
- Predictive analytics reduces readmissions by up to 25%, helping hospitals anticipate demand and allocate staff.
- Automation tools slash billing backlogs by 50%+, freeing clinicians from administrative drag.
- The future is connected AI: integrating data from EHRs, wearables, and imaging to deliver proactive, personalized care.
- Winning strategy: start small, prove ROI fast, and scale what works.
What Is the Future of AI in Healthcare? Let’s Understand the Historical Context First
The future of AI in healthcare is about making care more personal, predictive, and practical. AI technology is learning to tailor treatments to each patient, sharpen diagnostics, and handle the repetitive work that eats up everyone’s time. It’s becoming a co-pilot for healthcare professionals, helping with decisions, guiding surgeries, supporting research, and keeping patients connected through telemedicine and wearable tools.

Historical Context
When people think of AI in healthcare, they usually picture robots in surgery or computers reading scans like seasoned doctors. But that’s not how it started. From 2010 to 2023, AI went from basic automation to technology that now supports how clinicians think, plan, and treat patients.
Let’s look at how AI has moved from pilot projects to the systems quietly running care every day:
Early 2010s
AI started small, handling scheduling, billing, and digital records. The goal was never to replace people but to make their days a little less buried in paperwork. Those early systems built the digital backbone that everything else now runs on.
Mid-2010s
Then came the big leap. Deep learning, a form of machine learning that recognizes patterns, changed medical imaging forever. After breakthroughs in computer vision around 2012, AI models started spotting signs of disease in X-rays and MRIs with impressive accuracy. In 2016, Arterys earned FDA clearance for a cloud-based deep learning tool that cut cardiac MRI analysis time from about 36 minutes to 6. By 2018, 13 AI-powered devices had FDA approval, proof that AI had moved from lab experiments into real-world use.
Early 2020s
The next shift came when AI started making sense of the messiest data in healthcare: notes, lab results, diagnostic images. About 80 percent of medical data is unstructured, and with natural language processing (NLP), AI learned to read it. That opened the door to predictive analytics. Hospitals began using AI to flag high-risk patients, anticipate readmissions, and plan staffing with more precision.
Those moments turned the use of AI from experiment to essential across the healthcare sector. The AI medical imaging market alone is expected to reach $19.78 billion by 2033, signaling how deeply it’s woven into modern care.
Current State Analysis
Today, AI is part of healthcare’s daily rhythm. It’s built into how hospitals schedule patients, track data, and make clinical calls. Let’s see what it’s like across healthcare:
- Adoption: By 2024, 71% of hospitals in the United States were using predictive AI tools connected to their EHRs, up from 66% the year before. Among physicians, adoption rose from 38 to 66%.
- Patient Engagement: Virtual assistants now book appointments, answer common questions, and handle basic triage within digital health portals used by primary care and specialty clinics.
- Predictive Analytics: Hospitals use AI to get ahead of crises. At the University of California San Diego, the COMPOSER system predicts sepsis risk and has helped reduce mortality by 17%. These systems run data analysis on EHRs and spot trouble before it shows up in vitals.
- Administrative Efficiency: AI is cutting down the paperwork that bogs everyone down. Auburn Community Hospital cut billing backlogs by 50% and boosted coder productivity by 40 percent using AI-driven tools.
AI has become the quiet engine behind modern healthcare that connects departments, improves accuracy, and unlocks new capacity without adding staff. And it’s already setting the stage for systems that learn across entire networks, not just single hospitals.
Emerging Capabilities
The next wave of AI in healthcare connects everything, from the first checkup to post-care monitoring. These tools aren’t just smarter; they’re more connected, practical, and patient-focused:
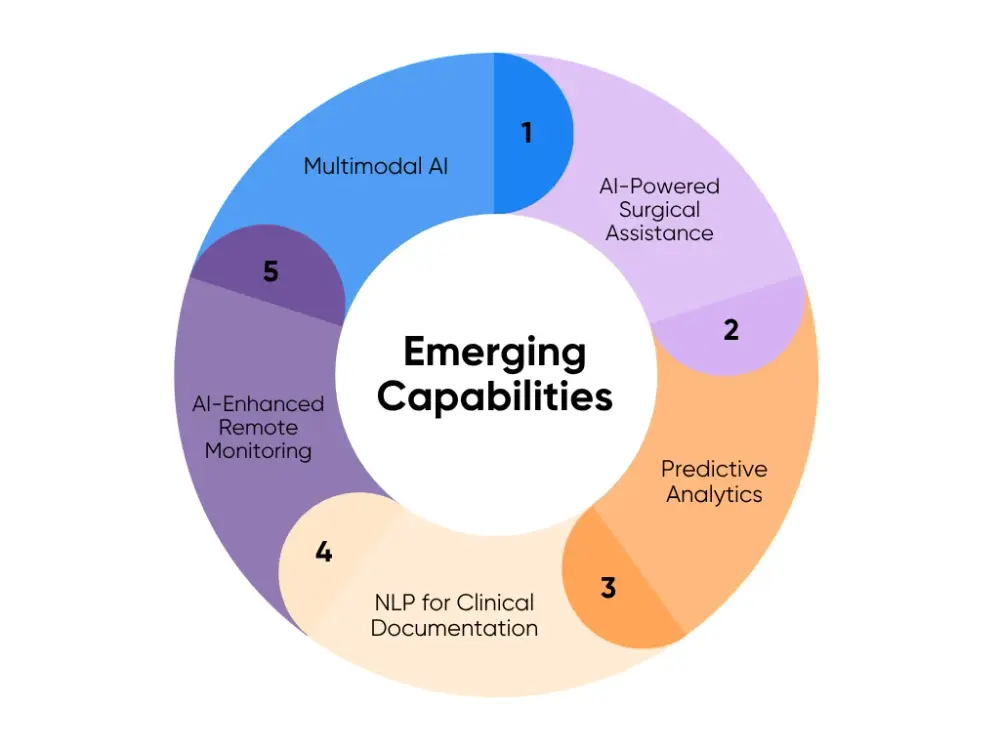
- Multimodal AI for Precision Medicine: AI now pulls together medical images, genomics, health records, and wearable data. That mix helps doctors understand each patient’s unique health profile and build treatment plans made just for them.
- AI-Powered Surgical Assistance: Inside the OR, AI algorithms guide surgeons in real time and connect with approved medical devices to improve precision. Fully autonomous surgery is still far off, but AI-assisted precision is already helping patients recover faster and safer.
- Predictive Analytics for Chronic Disease Management: AI watches data from wearables and sensors to spot early warning signs in patients with chronic conditions like diabetes and heart disease. It alerts care teams before things worsen, reducing emergency visits and keeping patients healthier at home.
- NLP for Clinical Documentation: AI reads through clinical data and extracts key insights instantly. No more scrolling through endless text. Clinicians see what matters most right away. That means faster, more accurate decisions and better patient outcomes.
- AI-Enhanced Remote Monitoring: Remote care powered by AI lets providers monitor patients’ vitals 24/7. If something looks off, the system alerts staff so they can act early. Patients recover safely at home, and hospitals save valuable capacity for those who truly need it.
As these tools mature, healthcare leaders, especially in mid-sized organizations, can use AI as a long-term growth strategy, not just a tech upgrade. Start small. Keep integration simple. Let AI strengthen what your teams already do well, and build from there.
Now that we’ve looked at how AI got here, let’s talk about where it’s heading next. Three big trends are shaping how healthcare teams will use AI through 2026, and how they’ll turn innovation into everyday impact. And no, it’s not all hype. This is where things start getting practical.
Trend #1: AI-Powered Diagnostic Enhancement
AI-powered diagnostic enhancement is changing how clinicians detect disease. It learns from scans, lab results, and notes to flag risks, rank urgency, and recommend next steps, all while keeping the clinician in charge. The goal is simple: faster reads, fewer misses, and more consistent results across teams.
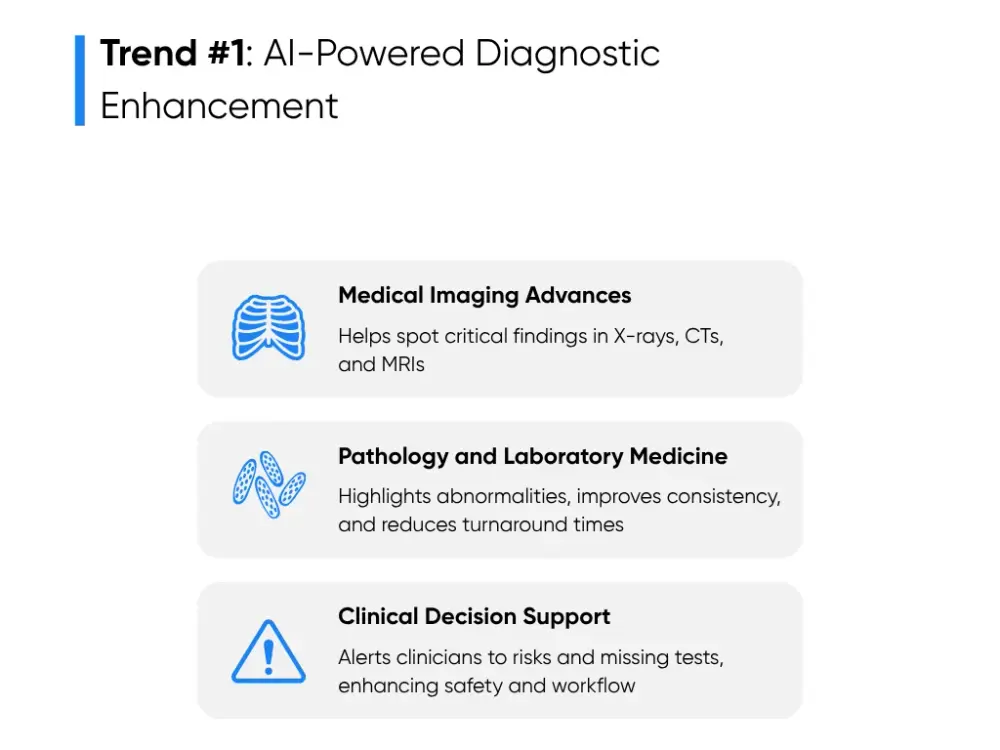
Here’s how that’s taking shape across imaging, pathology, and clinical decision support:
Medical Imaging Advances
AI in medical imaging can perform preliminary reviews of X-rays, CTs, and MRIs. These can assist radiologists in screening for breast cancer, detecting lung nodules, and flagging fractures or pneumonia.
Studies show that AI applications can now match or even exceed human readers in accuracy, reaching around 0.90 AUC in mammography and other high-volume imaging tests. That consistency helps teams catch early-stage disease and act faster when timing matters.
Imaging AI pays off in two ways:
- Triages cases automatically and pushes critical scans to the top of the queue.
- Reduces rereads between radiologists.
Hospitals that integrate imaging AI report faster reads (often cutting turnaround times by double digits) and fewer delays for patients waiting on results.
The smartest way to roll it out is to plan integration early. Connect the model to PACS and EHR systems so overlays, heatmaps, and notes appear in the tools your radiologists already use. Start small with a single use case, like chest X-ray triage, and measure results for 60 to 90 days. Track metrics like accuracy, read time, and additional testing rates.
Smaller hospitals can begin with a per-study pricing pilot, while larger systems can move to annual or volume-based licensing once proven.
Pathology and Laboratory Medicine
Pathology AI looks at whole-slide images and highlights regions worth a closer look. It can count cells, grade tumors, and identify irregularities that might be missed in manual reviews. In clinical labs, AI models classify blood cells, check for outliers, and validate results before release. The aim is to take on the repetitive work and make sure specialists focus their attention where it’s needed most.
Research shows pathology AI improves consistency between readers and reduces variability in diagnoses. Turnaround times drop once slides are scanned and queued by AI. Labs see steadier quality, fewer discrepancies, and faster case sign-outs.
For smaller hospitals, the entry point is digitizing slides through a partner and using cloud-based AI. Start with a high-volume specialty like prostate, breast, or hematology. Larger systems can embed AI directly into their laboratory information systems (LIS) so predictions and alerts flow into technician dashboards.
Expect to budget for slide scanners, data storage, and model validation. Cloud delivery lowers upfront costs and speeds up deployment. Over time, savings come from fewer repeat tests, shorter processing times, and tighter lab staffing.
Clinical Decision Support
Clinical decision support (CDS) brings AI insights right into the EHR. It reads real-time data, monitors vital signs, and triggers alerts for potential issues. It might recommend a missing test, warn about drug interactions, or flag early signs of sepsis or heart failure. The clinician still makes the decision; AI just adds context at the right moment.
Evidence shows that well-designed CDS systems improve patient safety and cut medication errors when they’re tuned to fit local workflows. The value comes from precise, relevant alerts, not endless pop-ups.
Each alert should have a clear purpose, an owner, and a one-click action such as an order set or note template. Keep insights where clinicians already work: on the same screen as orders and charting.
To start, mid-sized hospitals can test one module, such as sepsis detection or readmission risk, in a 60-day silent pilot. Use that period to fine-tune thresholds and confirm that alerts align with workflow before going live.
Implementation at any size follows the same playbook:
Pick one diagnostic workflow with clear volume and pain.
Plug the AI into the systems your team already uses.
Track accuracy, turnaround, follow-up actions, and patient outcomes.
Train a few super-users early, then publish quick wins to build buy-in.
AI doesn’t need to replace how you work; it should make your team’s work sharper and faster. Start focused, prove the results, and scale what works. That’s how AI delivers ROI and lasting clinical value without disrupting care.
Trend #2: Predictive Analytics and Population Health
Predictive analytics is helping healthcare teams anticipate better. AI is good at finding patterns in patient data and guiding smarter care decisions. For mid-sized hospitals, it’s a way to manage resources better, keep chronic patients stable, and stay a few steps ahead of the next emergency.

Think of predictive analytics as the weather forecast for patient care. It studies health data from EHRs, labs, wearable devices, and claims, then predicts what might happen next. It can flag who’s at risk for sepsis or heart failure, identify patients likely to skip appointments, or forecast a spike in ER visits after flu season. The goal isn’t to predict everything. It’s to give care teams enough lead time to act before problems get serious.
Hospitals use these insights to plan staffing, adjust capacity, and focus outreach where it matters most. Instead of scrambling when the waiting room fills up, they already know what’s coming and have the right people in place.
Predictive analytics delivers strong results in a few key areas:
- Readmission Reduction: AI scans discharge notes, vitals, and follow-up data to predict which patients might return within 30 days. A quick nurse call or home visit can prevent that. Some systems have cut readmissions by up to 25%.
- Chronic Disease Management: AI keeps tabs on long-term conditions like diabetes or COPD. When a wearable shows small but worrying changes, like higher resting heart rates or blood sugar spikes, it alerts care teams before the patient needs the ER.
- Operational Forecasting: Hospitals use predictive models for patient monitoring, staffing, and bed use. By analyzing admissions and seasonal patterns, AI helps reduce wait times and smooth out the daily chaos of patient flow.
- Population Health Planning: Public health teams use AI to spot trends across communities, like rising asthma or low vaccination rates. That helps them focus prevention efforts before cases surge.
Mid-sized organizations can adopt predictive analytics in stages:
Clean and connect data: Start by combining EHR, claims, and lab data in one secure platform. Inconsistent or incomplete data leads to unreliable predictions. A connected data foundation is non-negotiable.
Start small and measurable: Choose one clear problem, like readmissions or chronic care follow-up. Small pilots build credibility and give teams time to learn before scaling.
Integrate predictions into daily workflows: Make predictions visible where end users already work, directly inside discharge planners, dashboards, or patient lists. If staff have to open another app, adoption will lag.
Test, measure, and tune: Track accuracy, intervention rates, and patient outcomes. Refine models as new data comes in and expand once results prove consistent.
Scale what works: Once a pilot succeeds, roll out to new departments or patient groups. Build a cross-functional AI task force with IT, clinical, and operations leaders to guide growth.
AI only works as well as the data it gets. Missing fields, inconsistent coding, and siloed systems can throw off results. Before rolling anything out, standardize data formats and ensure data privacy and HIPAA compliance across all healthcare data sources.
Integration can be tricky, too. Many hospitals use multiple systems that don’t talk to each other. You can embed predictive analytics directly into the EHR so results appear alongside patient notes, care plans, or discharge checklists. When insights are visible in real time, teams can act immediately instead of sifting through separate reports.
Also, that’s where we help. At Aloa, we build AI systems that integrate smoothly into existing workflows, without unnecessary or complex add-ons. We work with hospitals to connect data sources, ensure HIPAA-safe environments, and deliver predictive models that fit day-to-day operations.
Trend #3: Administrative Automation and Operational Efficiency
Hospitals run on their established systems. But those legacy systems can get bogged down by paperwork, scheduling, and endless coordination. AI is starting to lighten that load for healthcare providers by automating high-volume administrative tasks.
Here's how hospitals are cutting costs, reducing errors, and getting more time to focus on patients:
Revenue Cycle Optimization
For most hospitals, the revenue cycle (everything from registration to final payment) is where money leaks out. AI helps close those gaps.
AI tools review and code claims before submission, flagging missing details, incorrect codes, or duplicates in minutes instead of days. Some hospitals report up to 70% fewer manual claim reviews. At Auburn Community Hospital, AI cut outstanding claims by 50% and boosted coder productivity by 40% within a few months.
Automation also speeds up slow steps like eligibility checks and prior authorizations, helping reduce delays that frustrate patients and slow revenue. Hospitals using AI for these tasks have shortened revenue cycles and improved cash flow reliability.
You don’t need to rebuild your systems to start. AI tools can plug into your existing EHR and billing software. Most hospitals begin with a cloud-based pilot (claims scrubbing or charge capture) costing $50,000 to $150,000. These pilots often pay for themselves within months through faster reimbursements and fewer denials.
Workflow Automation
Workflow automation helps admin teams get ahead of the daily grind. Whether it’s filling the schedule, managing shifts, or tracking resource use, AI brings data and action together in real time.
Let's see how hospitals are using AI to make everyday operations run smoother:
- Scheduling: AI studies patterns (no-shows, cancellations, patient flow) and fills open slots automatically. When linked to patient portals, these tools can send reminders or rebook cancellations automatically.
- Staff Management: AI analyzes patient volume and shift trends to balance workloads. Instead of guessing where coverage might fall short, it suggests optimal staffing and flags issues before they become crises. This keeps care teams supported without overspending.
- Resource Allocation: AI tracks how ORs, imaging machines, and other assets are used. When it spots idle time or scheduling conflicts, it adjusts automatically to maximize uptime. That improves data management and reduces idle time.
To get started, you can pilot one function, such as appointment scheduling or nurse staffing. The key is to keep integration simple. Connect AI to the tools already used for scheduling or HR management, then expand across departments once results are clear.
Patient Experience Enhancement
AI is also improving how patients experience care, from the moment they schedule an appointment to post-visit follow-up. It removes friction, shortens wait times, and keeps communication consistent.
Here’s how AI is reshaping each step of the patient journey:
- Virtual Support: Chatbots and assistants handle routine questions like appointments, reminders, and insurance info 24/7. Hospitals using them report up to a 30% increase in patient interactions, which improves care adherence.
- Faster Check-Ins and Feedback: AI-powered kiosks and portals simplify registration, cut paperwork errors, and gather post-visit feedback automatically. Sentiment analysis then highlights recurring issues so teams can fix them early.
- Personalized Follow-Up: AI flags patients likely to miss follow-ups or need extra help. That way, staff spend their time where it counts, on patients who need it most.
For your organization, start small with automated reminders or chatbot support that connects to your current communication systems. These tools are affordable, easy to deploy, and show quick gains in patient satisfaction and retention.
At Aloa, we help healthcare organizations put AI automation into action. From revenue cycle pilots to full workflow integration, our goal is to make your systems work smarter, so your teams can focus on better care.
What to Consider if You Want to Implement AI in Healthcare?
AI is becoming part of everyday healthcare. But success depends on how you plan, not just what you buy. Too many hospitals rush in without clear goals or structure and end up with tools that don’t deliver.
The real aim isn’t to “do AI.” It’s to make work smoother, care better, and results measurable. Here’s how to start smart:
Assessment and Planning
Before you invest in AI, take stock of where you are. A readiness assessment helps you understand your current systems, data quality, team skills, and budget.
Ask three simple questions:
Where do we lose the most time or money?
Where do errors or delays keep happening?
What data do we already have that could help fix these problems?
The answers point you to the best starting place, like billing automation, scheduling, or readmission prediction. Focus on one measurable goal first. It’s easier to show value and build momentum from there.
Once you’ve picked your use case, create a short plan. Keep it clear and collaborative:
- Set goals: Define what success means (for example: 15% faster claims, 10% fewer readmissions).
- Check your data: Make sure it’s accurate, complete, and secure.
- Plan the timeline: Start with a short pilot before expanding to reduce risk and pace the adoption of AI across teams.
- Confirm compliance: Every step should meet HIPAA and security standards.
At Aloa, we guide healthcare teams through this process, from readiness assessment to pilot design, so you can move from concept to measurable results with less risk.
Implementation Best Practices
Once the plan is ready, focus on how AI fits into your daily workflow. It should support your team, not disrupt it.
Here’s what works best:
- Choose compatible tools: Look for systems that integrate with your existing EHR or billing software. Avoid big rebuilds; modular tools for tasks like scheduling, coding, or risk prediction can show value fast.
- Train your team: Short, focused sessions go further than long tutorials. Show how AI saves time and reduces hassle.
- Start small: Run a 60–90 day pilot, measure outcomes, and refine. Focus on metrics that matter, like turnaround times, denials, or staff hours saved.
- Communicate clearly: Keep teams informed about why AI is being introduced and how success will be measured. Celebrate small wins and share numbers openly to build trust.
AI implementation doesn’t have to be complex. With the right partner, it’s a straightforward upgrade. Aloa’s AI integration and automation services are designed to fit your existing operations so you see results fast, without disruption.
Future-Proofing Strategies
What works now may look different two years from today. Staying ready means building flexible systems that can grow with you.
A few key habits keep your investment relevant:
- Pick flexible platforms: Use AI platforms that allow updates and add-ons instead of one-off solutions. Cloud-based systems make it easy to add new models or expand to new use cases.
- Maintain data quality: Keep your data organized, consistent, and secure. Clean data is what keeps your AI accurate.
- Track and tune: Review performance regularly and retrain models when patient populations or workflows change.
- Stay current: Keep an eye on emerging trends like multimodal AI, NLP, and predictive analytics for drug development in life sciences. They’ll shape how care is delivered in the near future.
At Aloa, we help hospitals future-proof their systems through ongoing support and optimization. Our healthcare AI solutions evolve with your workflows, regulations, and technology so you’re always a step ahead.
AI in healthcare is about smarter operations and better outcomes. When you start with clear goals, clean data, and a solid plan, AI becomes more than a project. It becomes a long-term advantage for your patients, your staff, and your organization.
Key Takeaways
AI isn’t the future of healthcare. It’s already part of it. The real opportunity now is smart adoption. Start small. Pick one measurable problem, automate it, prove value, and grow from there.
At Aloa, we help organizations shape the future of AI in healthcare one project at a time. From AI implementation to workflow automation and custom AI solutions, we make it practical, secure, and scalable.
If you’re exploring AI or deciding where to begin, let’s talk. Tell us your biggest challenge. We’ll help you turn it into a clear, results-driven plan.
Join our AI Builder Community on Discord or subscribe to our Byte-Sized AI Newsletter for insights, tools, and updates that help you stay ahead.
FAQs About the Future of AI in Healthcare
How will AI in healthcare change from 2025 to 2026?
AI is shifting from small tests to full use across hospitals. It’s moving from helping with tasks to driving entire workflows (still with human oversight). You’ll see AI connecting text, images, and data in one view, supporting both treatment planning and home-based care. By 2026, most teams won’t be asking if they should use AI, but how to make it better.
How much should healthcare organizations budget for AI?
Budgets are growing fast. Most health systems now spend 5–10% of their tech budgets on AI. Diagnostic and analytics tools usually run $200K–$1M. Larger automation programs can reach $2M. Smaller teams can start with $50K–$200K pilots using cloud-based tools. Think of AI as a long-term investment, not an extra expense.
Can smaller organizations afford AI?
Yes. Cloud AI platforms and software subscriptions have leveled the field. Smaller hospitals can use enterprise-grade AI for $50K–$300K a year. They can roll out diagnostic tools, predictive models, or workflow automation without heavy infrastructure. Strategy and good planning matter more than size.
How should healthcare leaders prepare for AI?
Start by checking your data. It needs to be clean, structured, and secure. Set clear goals and ROI targets before choosing a tool. Get leadership support, train staff early, and build teams that mix clinical and technical skills. Spend time planning how AI fits into your daily workflow before turning it on.
How can organizations future-proof AI investments?
Pick flexible tools that integrate with new tech. Focus on strong data systems that can support many AI uses, not just one. Train your team so you’re not relying only on vendors. Review your systems often and update as needed. AI evolves fast, and staying current keeps your investment valuable.