Healthcare runs on speed and trust. While the benefits of AI in healthcare are showing up in fewer misses, faster care, and smarter use of every hour, the real question is how you can build AI into your operations in a way that earns speed and trust.
That’s where we focus on at Aloa. We help healthcare teams build AI systems that work in real clinics, on real timelines, under real pressure. From imaging and prediction to workflow automation and clinical support, we design tools that are HIPAA-compliant and can prove their value quickly.
Here’s what this guide covers:
- Quick wins to act on now: imaging, prediction, and automation
- Long-term plays to plan for: personalized care, virtual health, and patient engagement
- Built-in guardrails for scaling: privacy, bias, and adoption
- ROI checkpoints that tie outcomes to cost and efficiency
You’ll walk away knowing exactly where to start without compromising patient experience.
How Is AI Improving Healthcare?
AI can improve care by speeding up diagnoses, predicting risks earlier, and personalizing treatment. The benefits of AI in healthcare also include automating admin work, delivering decision support, and helping researchers test new drugs faster. It powers remote monitoring tools that track recovery and flag issues before they turn into emergencies.
Walk through any hospital today, and you’ll see AI already at work:
- Radiology teams catch diseases earlier with AI-assisted imaging.
- Clinicians predict which patients may decline before it happens.
- Administrators finally see workflows that don’t swallow half the day.
- Researchers accelerate medical research and drug development faster than ever.
Each application of AI shares one goal: to turn data into actions that can improve patient care.
And right now, the biggest improvements are coming from:
- Imaging analysis that boosts accuracy for disease diagnosis.
- Predictive analytics that flag risks early.
- Automation that clears low-value tasks.
- Personalized treatment built on real-time data.
- Drug discovery tools that shorten R&D cycles.
- Remote monitoring with wearable devices that keep care connected post-discharge.
- Patient experience platforms that make communication and access easier.
We’ll explore these different ways AI is transforming healthcare in detail below.
1. Enhanced Diagnostic Accuracy Through AI Imaging Analysis
AI can break medical scans down into pixels, comparing them to millions of labeled images in a short amount of time. A faint shadow on a lung X-ray or a slight density change in a CT scan can change the diagnosis. And what used to take hours now takes minutes.
You see this specific impact most clearly in radiology and pathology, where speed and accuracy directly affect health outcomes. Similar trends are emerging across hospital operations.
Radiology Applications
AI algorithms trained on millions of scans now review X-rays, MRIs, and CTs in seconds, flagging issues with accuracy that rivals top specialists. Here’s how:
- X-rays: AI detects pneumonia, fractures, and TB with over 90% accuracy. In the ER, it can flag a possible infection before the radiologist even opens the file, cutting time-to-diagnosis from hours to minutes.
- MRIs: NYU Langone Health built fastMRI, an AI system that produces high-quality MRI scans using one-fourth the data of standard imaging. Scan times are cut by more than half, which means quicker results and smoother patient flow.
- CT Scans: In cardiology and oncology, AI highlights tiny nodules or blocked arteries that could signal early cancer or heart disease. That gives care teams time to intervene sooner and avoid escalation.
Pathology Innovations
In pathology, the shift has been as powerful. Instead of spending hours under a microscope, pathologists now review digital slides pre-screened by AI. For context:
- Breast Cancer: AI-assisted slide reviews match expert-level accuracy (above 95%) while cutting review time nearly in half. Flagged slides show where to focus.
- Prostate and Skin Cancer: Models trained on thousands of confirmed cases can catch subtle malignancies that even experienced eyes might miss.
- Beyond Detection: Some deep learning algorithms go further, grading tumor aggressiveness and predicting patient outcomes based on cell structure. That gives oncologists stronger data for treatment planning.
The biggest gain here is reliability. Every slide gets the same close read, every time. AI can act as a guardrail against human errors, ensuring even more accurate diagnoses.
Implementation Success Stories
Here are hospitals already using AI imaging and seeing measurable results:
- Mayo Clinic uses AI models that detect early signs of heart disease from ECG data, even from smartwatches. One model identifies weak heart function without a CT or MRI, giving clinicians faster insight into cardiac risk.
- Mass General Brigham developed Sybil, an AI tool that predicts lung cancer risk from a single low-dose CT scan with up to 94% accuracy. It spots patterns invisible to the human eye, helping radiologists focus on high-risk patients sooner.
AI imaging shows how small, smart workflow changes deliver real impact.
2. Predictive Analytics for Preventive Care
This is a huge-if-true moment: AI is starting to predict what kind of care patients will need based on their risk profile. AI can help flag people at risk for things like heart attacks, diabetes complications, or hospital readmissions. Incorporating AI can also help create a more interactive, user-friendly experience for patients to update their family medical history.
Today, many high-risk patients rely on outdated self-report surveys to keep their doctors informed. It’s not sustainable for hospitals to manually remind every patient to complete self-reported risk assessments, such as breast cancer screenings, before reaching a certain age.
AI can play the critical role of transforming care from reactive to preventive, helping providers act early.
Risk Assessment Models
At the core of predictive AI is risk modeling. These tools use past data (labs, vitals, prescriptions, demographics, even clinical notes) to estimate how likely someone is to develop a condition or face a complication. It’s not guesswork. It’s math built on thousands (or millions) of patient records.
Here’s how different models work:
- Logistic Regression: The simplest kind. It uses variables like blood pressure, BMI and age to calculate risk of something like heart disease.
- Random Forests / Gradient-Boosted Trees: These can process hundreds of variables at once and rank patterns linked to future outcomes.
- Neural Networks: These go further. They analyze unstructured data such as clinical notes or images alongside labs. Some models flag very early risk, even in cases that look low risk by traditional scores.
One widely used model is Epic’s sepsis prediction algorithm, which monitors electronic health records data and alerts clinicians when a risk score hits a critical level. Some hospitals using it have cut sepsis mortality by up to 44%.
Another example: Cleveland Clinic researchers developed a machine-learning model to assess cardiac risk in cancer patients, identifying markers and subgroups that traditional models miss.
Patient Monitoring Systems
Picture a heart failure patient wearing a remote monitor that tracks heart rate, weight, and oxygen levels. That data flows to an AI system trained to recognize warning signs: weight gain, labored breathing, or lower blood oxygen. If those patterns line up, the system sends an alert (sometimes before the patient even feels worse).
Some examples already in use:
- Current Health and Biofourmis use wearables and home sensors to track patients with chronic illness. Their AI flags early deterioration and alerts care teams.
- EarlySense, used in hospitals, monitors subtle movements and vital signs from under-mattress sensors. It helps nurses catch respiratory issues or fall risks before they escalate.
This is preventive care that works. It keeps patients out of the ICU, reduces readmissions and length of stay, and gives clinicians a way to act before a crisis hits.
And now, many health systems are starting to combine predictive risk scores with live monitoring. That means a patient’s risk profile updates constantly based on real-time data.
3. Streamlined Administrative Operations
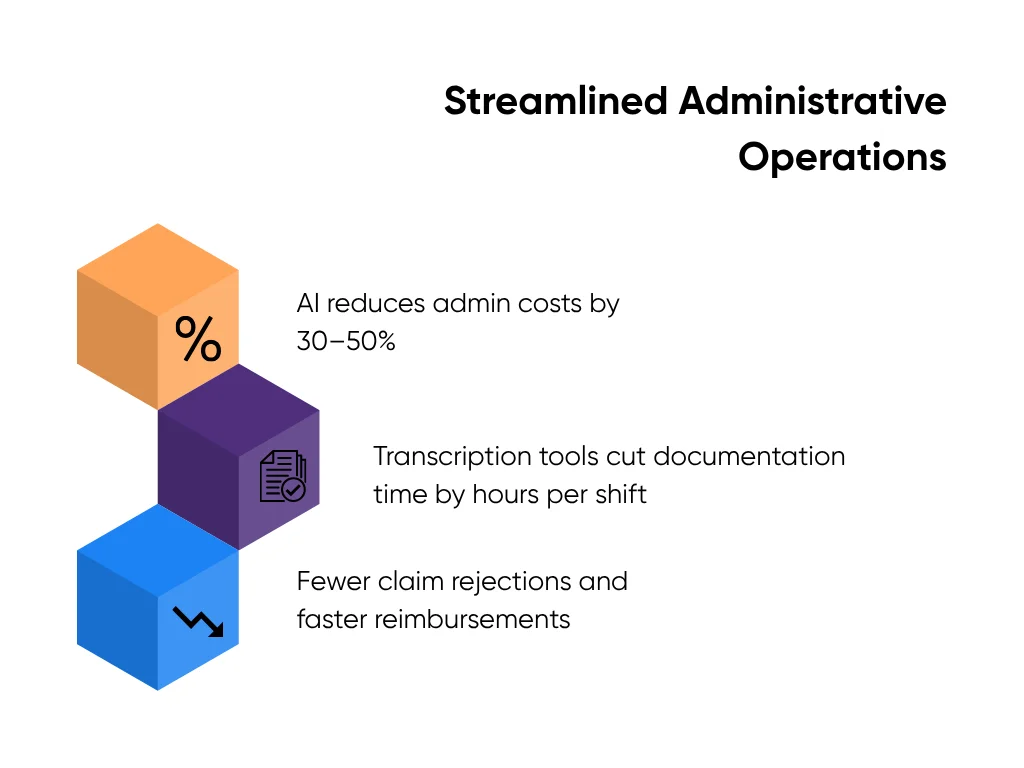
Paperwork slows your operation. Scheduling, billing, and documentation pull time away from patient care. These are workflow problems, not clinical ones. AI is great at handling repetitive administrative tasks so your staff can focus on people instead of screens.
Here’s where AI is making a visible difference in back-office operations:
Patient Intake and Registration
AI speeds up check-in by pulling patient demographics and insurance details from IDs and payer systems. It flags mismatches early so staff don’t have to re-enter data or chase missing forms. Clinics that automate intake often see shorter lines, fewer claim rejections, and smoother billing downstream.
Clinical Documentation and Coding
Documentation slows every provider. AI removes that drag. It uses speech recognition to listen, transcribe, and build structured encounter notes ready for coding and billing. Our HIPAA-Compliant Medical Transcription Tool shows how this works in clinical practice. It captures dictation, generates clean transcripts in seconds, and structures them for coding accuracy. Teams using this kind of automation consistently report shorter documentation cycles and cleaner billing records (time that goes straight back to patient care).
Claims and Denials Management
Billing teams lose hours correcting small errors. AI finds them faster. It checks each claim for completeness, aligns codes with payer policies, and flags likely denials before submission. Staff fix problems early, so clean claims go out the first time. This kind of automation helps cut rework, speed up reimbursements, and improve resource allocation without expanding headcount.
Scheduling and Capacity Optimization
AI studies appointment patterns to predict no-shows, fill gaps, and balance provider workloads. It keeps calendars full without adding manual coordination. Clinics that use automated scheduling often see steadier patient flow, fewer overtime hours, and faster turnaround between visits. Patients get seen sooner, and staff finish shifts on time.
All of the applications above will have to work with your existing workflow and will require some changes to your staff’s workflow. It’s also important to ensure that any technological transformation you undertake correctlyy handles Protected Health Information (PHI). Our guide, How to Make Any AI Model Safe through HIPAA Compliance, breaks down how to secure data, limit access, and track every action so you can automate responsibly.
4. Personalized Treatment Planning
Personalized treatment planning uses a patient’s unique data, like lab results, scans, and medical history, to create a treatment plan tailored specifically for them. AI analyzes this data, spots patterns, and provides clinicians with the insights they need to make faster, more accurate decisions.
It delivers evidence almost instantly, something that would normally take hours to find manually. Here’s how AI technology speeds up care and enhances decision-making:
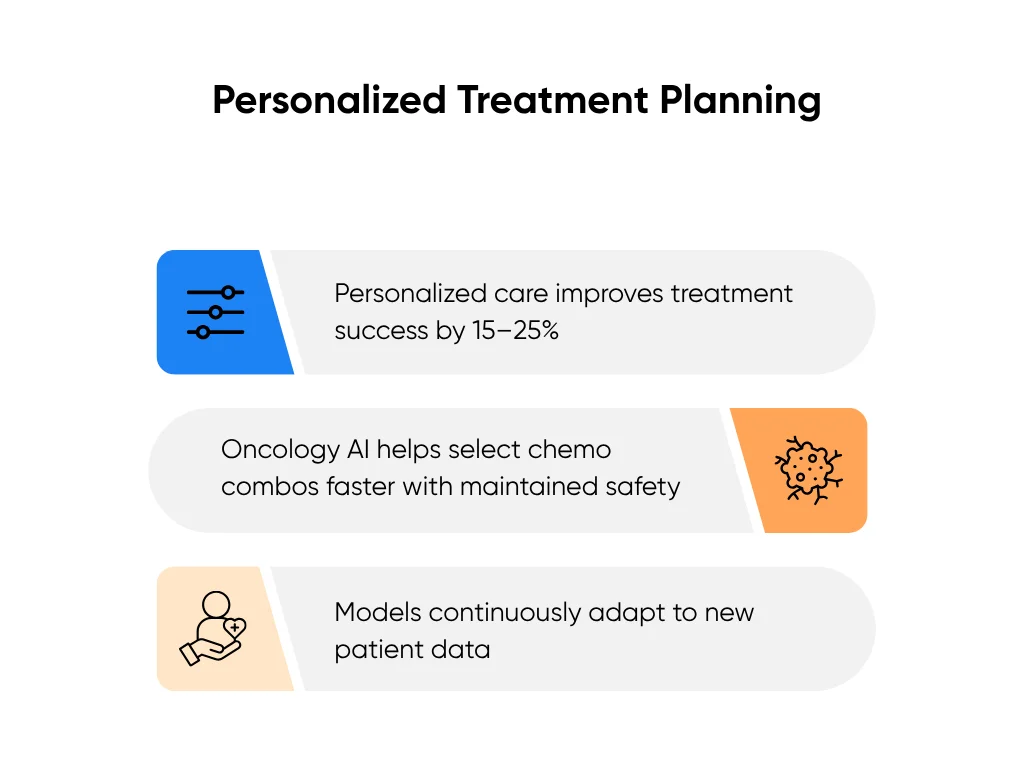
Data Analysis Methods
AI starts with data. It pulls information from health records, lab results, imaging, and devices, then organizes it so it can be compared and analyzed. Machine learning models find links between symptoms, test results, and outcomes. They highlight which factors matter most for each condition and show how similar patients responded to different treatments.
That means your team can base decisions on thousands of prior cases, not guesswork. BMC Medical Education notes that AI-driven data analysis already helps clinicians match treatments to patient subgroups more accurately than manual review.
Treatment Optimization
Once data is ready, AI models, called personalization algorithms, suggest what’s likely to work best for a specific patient. These algorithms study outcomes across many cases and learn which treatments succeed under which conditions.
For example, AI may find that patients with a certain heart rhythm respond better to one drug than another. It gives healthcare professionals ranked options backed by data. When patient results shift, the model updates its prediction.
This approach shortens trial-and-error cycles, reduces side effects, and helps patients reach stable outcomes faster. It also saves time for clinicians, who spend less effort revisiting old cases or searching for best-fit options.
Clinical Validation
Every model needs proof. Clinical validation tests AI’s recommendations against real-world results to confirm that they improve care. Hospitals run controlled pilots, measure changes in treatment accuracy and recovery rates, and adjust as needed.
BMC Medical Education highlights oncology studies where AI-supported planning helped clinicians select effective chemotherapy combinations faster without losing safety or accuracy.
The outcome isn’t machines replacing experts. It’s experts getting better data, faster.
AI can turn your patient data into direction your clinicians can act on. It helps them choose the right therapy sooner, skip trial-and-error steps, and deliver results faster.
5. Drug Discovery and Development
Bringing a new drug to market can take more than a decade. AI is helping shorten that timeline. It analyzes medical research for drug development using vast amounts of large data sets, predicts which compounds might work, and helps your scientists focus on the strongest options.
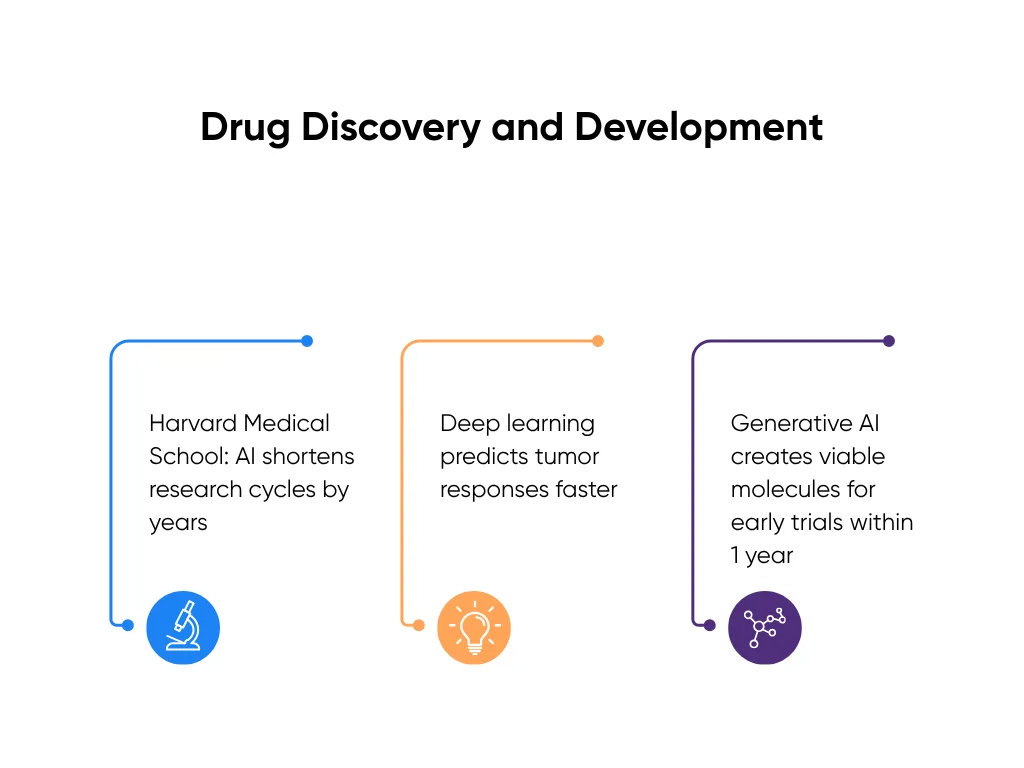
AI doesn’t invent cures by itself. It supports discovery across three main jobs, which are predicting, testing, and creating:
- Machine learning models predict how molecules behave. They study chemical structures, compare them to known drugs, and estimate how they’ll interact with target proteins or receptors. Instead of testing thousands of compounds manually, your team can use algorithms to narrow the list to a few promising ones.
- Deep learning algorithms go further. They use multi-layered neural networks (computer systems designed to recognize complex patterns) to simulate how molecules act inside the body. These models learn from thousands of test results and improve with every training cycle.
- Generative AI models create new molecular structures from scratch. They use patterns from existing compounds to design candidates that fit a target profile. Think of it as a digital collaborator that can explore millions of chemical variations before your team even starts synthesis.
These algorithms are already at work in real labs. Pharmaceutical teams use AI screening to drop weak compounds before testing. Deep learning models study tumor genetics to predict which cancer drugs have the best chance of success. Generative AI now designs new molecules that reach early trials within a year instead of five.
Harvard Medical School reports that these tools accelerate early research by finding viable candidates faster than traditional methods.. That means shorter discovery cycles and faster movement toward testing and approval.
Future Potential Applications
AI’s next step is connecting lab work with real-world clinical data. Large language models will use patient outcomes and population data to refine research in real time. This will help your teams:
- Predict how patients will respond before trials begin.
- Find new uses for existing drugs through repurposing.
- Build personalized drug combinations based on genetics and medical history.
AI will also strengthen post-market safety. Once a drug reaches patients, models can scan health records and flag potential side effects early, well before traditional reporting systems catch them.
AI isn’t replacing your research teams. It’s giving them faster feedback, cleaner data, and more shots that hit. When your discovery cycle speeds up, patients don’t wait ten years for new treatments. They see results in their lifetime.
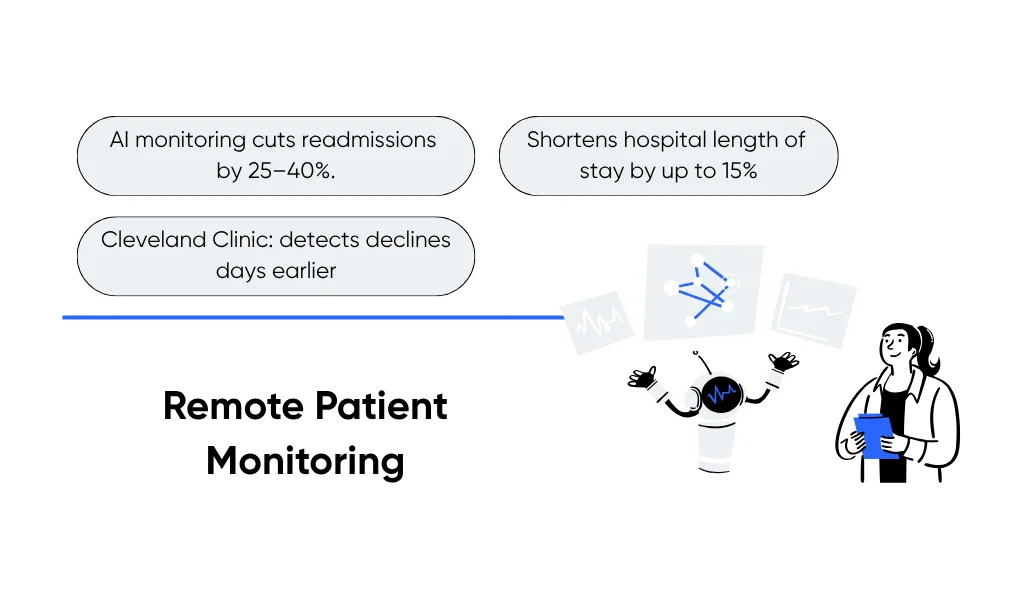
6. Remote Patient Monitoring
Remote patient monitoring combines connected devices with smart analytics to spot early warning signs, notify care teams, and prevent avoidable hospital visits. It’s simple in concept: collect real-time data, process it instantly, and act before a small issue turns into a serious one.
Let’s break it down:
Monitoring Technologies
Remote monitoring starts with the tools patients already use:
- Wearables like smartwatches, glucose sensors, and heart-rate trackers capture oxygen levels, blood glucose, heart rhythm, and sleep data. Each reading flows into secure dashboards your team can access in real time.
- Connected medical devices (digital blood pressure cuffs, ECG patches, or spirometers) add clinical-grade precision for chronic care programs.
- Smart home platforms integrate these readings, giving clinicians a full picture of the patient’s health without repeated visits.
For example, a patient with heart failure steps on a smart scale and gains two pounds overnight. That signal, combined with heart-rate data, suggests fluid retention. The AI system flags it immediately so your care team can call, adjust medication, and prevent an admission.
According to the Cleveland Clinic, hospitals using AI-supported monitoring identify health declines days earlier than traditional reviews. That means faster intervention and fewer ER visits.
Data Analysis Systems
AI gives all that data meaning. Thousands of readings arrive daily (far too many to check manually). AI systems handle the heavy lifting:
- Filtering and organizing data so only meaningful changes reach your dashboard.
- Machine learning models that detect anomalies like oxygen drops or irregular rhythms, sending alerts to the right person at the right time.
- Predictive analytics that study trends over time to forecast risk, such as readmissions or medication noncompliance.
When the system sees a patient trending toward danger, your team can adjust a treatment plan, schedule a follow-up, or send education material before a minor dip turns into a crisis.
Implementation Guidelines
Start small and plan for adoption of AI at each step:
- Choose one condition to monitor first, like diabetes or post-surgical recovery, where daily data adds immediate value.
- Pick interoperable systems that connect with your EHR to avoid manual entry and reduce friction for staff.
- Define clear alert protocols. Decide who responds, how alerts are verified, and what actions follow. This prevents alarm fatigue and ensures timely care.
- Prioritize compliance and security. Use HIPAA-compliant systems, encrypt all data, and set role-based access controls. Patients need to know their information stays private.
Once live, your clinicians gain a steady flow of insight instead of a flood of raw numbers. They see which patients need attention, when, and why, without extra steps or second-guessing. That’s when remote monitoring becomes part of care, not just another tool.
7. Enhanced Patient Experience
Good care doesn’t end with treatment. It’s how patients feel through the process that defines trust. AI helps your team deliver care that’s not only faster and safer but also easier to understand and stay connected to.
When AI works well, patients don’t see technology. They see responsiveness, clarity, and a sense that their care team never lost track of them. For more field-tested wins on access and communication, see our examples of AI in healthcare.
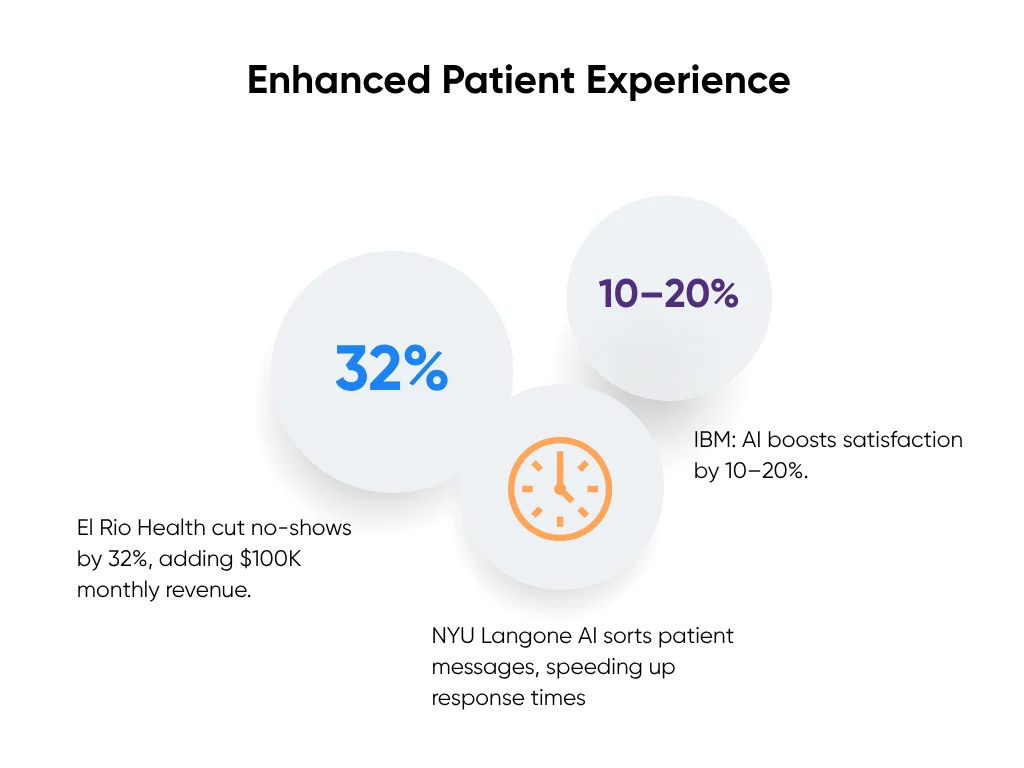
Patient-Centered Benefits
AI makes care feel personal again. It helps patients get answers quickly, understand their care plans, and stay on schedule:
- 24/7 virtual assistants handle simple questions, refill requests, and scheduling. Patients get instant help without waiting on hold. That responsiveness builds confidence and keeps your front desk from drowning in calls.
- Personalized communication tools tailor reminders and education based on patient data. Someone with diabetes, for example, receives nudges about glucose checks or meal planning (which are specific, actionable messages, not generic texts).
- Predictive follow-ups identify when a patient may need support before they ask. If blood pressure trends upward or medication refills drop, AI flags it so your staff can check in early.
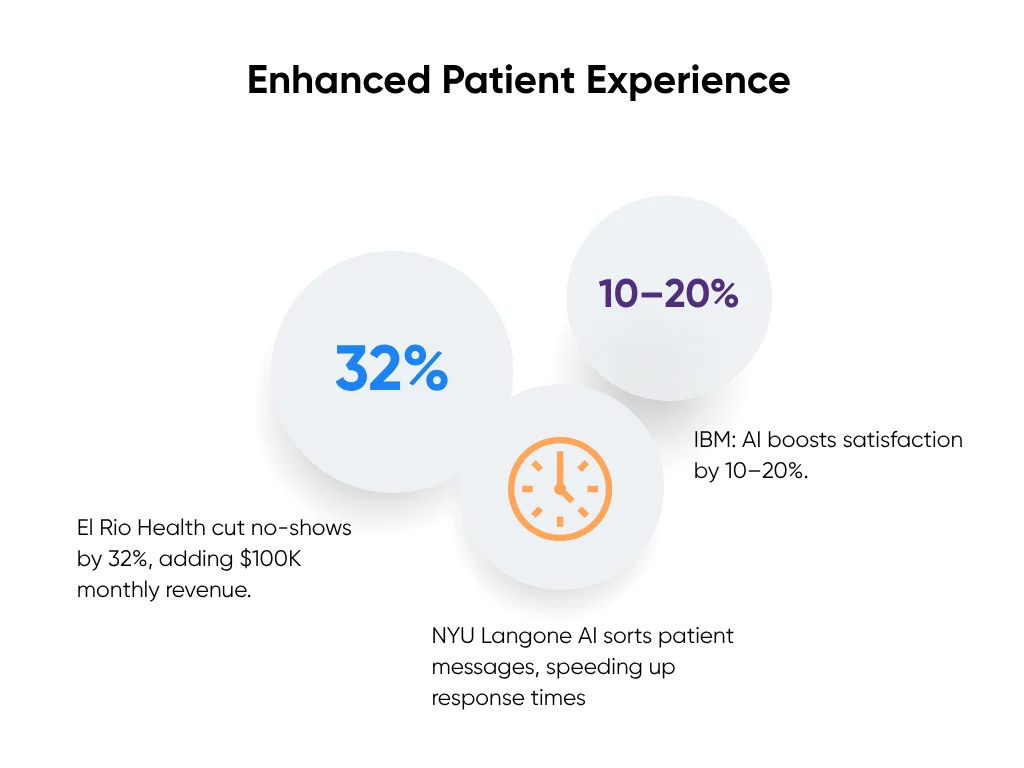
At El Rio Health, a community clinic network in Arizona, an AI reminder system cut appointment no-shows by 32% and added about $100,000 in monthly revenue after launch. The best part: patients came back for care they might have skipped.
Accessibility Improvements
AI removes barriers that stop patients from staying involved in their care:
- Language translation systems built on natural language processing turn clinical notes and discharge instructions into plain, native-language summaries. A patient who doesn’t speak English fluently can still understand every instruction.
- Voice-enabled systems with speech recognition guide patients through apps or telehealth visits without typing or scrolling. For someone with low vision or limited mobility, that’s the difference between independence and frustration.
- AI triage systems in telehealth platforms help healthcare organizations route patients to the right clinician faster, cutting unnecessary wait times and freeing up emergency departments.
According to IBM, AI tools that simplify communication and self-management directly improve patient satisfaction. When people understand their care and feel seen, engagement follows naturally.
Real-World Results
At NYU Langone Health, AI now helps sort thousands of patient-portal messages. The system spots urgent requests first, speeding up replies for patients who need help quickly. Staff call it a quiet but powerful fix that makes their days easier.
We’ve seen similar results in Aloa’s healthcare projects. When we build AI tools that match how patients really communicate (clear language, cultural fit, simple access), engagement naturally improves. People respond when the system feels designed for them.
AI doesn’t replace empathy; it amplifies it. It gives your team the tools to stay present even when they can’t be in the room. Patients notice that. They feel informed, supported, and valued. And that’s what lasting engagement looks like.
Key Takeaways
AI reshapes healthcare one workflow at a time. Clinicians diagnose faster, staff clear backlogs, and patients get answers sooner. The benefits of AI in healthcare show up where everyone’s watching: on the clock and in the budget.
Skip the “big transformation” story. Start small, fix what hurts most, and prove it works. One clean win beats ten PowerPoint promises. Stack a few of those, and momentum builds fast.
Keep the guardrails tight. Protect data like it’s your own. Check the math twice. Train your people until they stop calling it “the new system.” When they own it, it lasts.
We at Aloa build AI that performs in real clinics. If you’re experimenting with AI or figuring out where to start, let’s talk. Share your biggest challenge; we’ll help you turn it into something that ships and proves its worth.
Then keep the ideas flowing. Join our AI Builder Community on Discord or grab our Byte-Sized Newsletter for practical lessons and honest wins from teams building AI that actually delivers.
FAQs About the Benefits of AI in Healthcare
How is AI improving healthcare outcomes today?
AI improves accuracy, speed, and cost across care. Imaging tools raise diagnostic accuracy by 15–30%, with some passing 95%. Predictive models flag high-risk patients up to three days early, cutting complications by 35%. Automation cuts admin costs by 30–50%. Personalized care boosts treatment success by 15–25%. Remote monitoring lowers readmissions by 25–40%.
Does AI replace healthcare workers?
No. It strengthens them. AI handles screening, data work, and paperwork so clinicians can focus on patients. Radiologists using AI improve accuracy by 10–15%. Nurses supported by AI monitoring manage 20–30% more patients safely. The best systems pair human judgment with AI precision.
What ROI should healthcare teams expect?
Most see returns within 6–24 months. Imaging AI pays off in 12–18 months through faster reads. Automation breaks even within a year. Predictive tools return value in one to two years by reducing readmissions. Focused pilots can start near $100K; full platforms reach $1M+. Many reach 200–400% ROI when targeting high-impact areas.
How long does implementation take?
Simple admin tools deploy in 2–4 months. Imaging AI takes 4–8 months. Predictive analytics need 6–12. Multi-department rollouts run 12–24. Start with a 90-day pilot, prove value, then expand.

