AI is already diagnosing faster, predicting risks earlier, and reducing the paperwork that consumes every nurse’s hour. Pretty great, right? Until it’s not. Models still misread scans. Sensitive data slips through cracks. Some tools even add more clicks than they remove. Sorting out which ones actually help takes more patience than most teams have left.
At Aloa, we build AI that earns its spot on your floor. HIPAA-safe. Easy to plug in. Proven where it counts. From predictive analytics to workflow automation, we design tools that deliver results, instead of becoming another dashboard to manage. And yes, we’ve built a few dashboards before we learned that lesson.
So, here’s what’s coming your way:
- Concrete examples of where AI strengthens patient care and streamlines daily operations
- Straight talk on the disadvantages of AI in healthcare
- Practical fixes for common AI challenges in healthcare
- A simple roadmap for scaling what works
By the end, you’ll have a clear, grounded view of the pros and cons of AI in healthcare: what delivers, what disappoints, and how to move forward without tripping over the next “smart” tool.
TL;DR
- AI in healthcare improves diagnostics, speeds up risk prediction, automates admin work, and enhances patient experience. Hospitals using AI have seen 20–30% lower administrative costs and 15–25% higher diagnostic accuracy.
- Key benefits: better diagnostic precision, predictive care reducing readmissions by up to 30%, streamlined workflows, remote monitoring that cuts ER visits by 40%, and faster drug research cycles (months instead of years).
- Main challenges: data privacy, fragmented datasets, integration limits, clinician resistance, and high development costs.
- Solutions: encryption, pilot testing, interoperability, modular AI adoption.
- The pros and cons of AI in healthcare hinge on responsible innovation: balancing security, trust, and compliance.
- Aloa builds HIPAA-compliant, explainable AI systems tested with real doctors, improving care while fitting seamlessly into clinical workflows.
What is AI's Role in Modern Healthcare?
Artificial intelligence improves modern healthcare by speeding up diagnoses, predicting risks sooner, and personalizing treatment. As we look at the pros and cons of AI in healthcare, AI’s role is simple. It turns clinical data into actions your team can use right now. It reviews images, reads notes, studies patterns, and then points your clinicians to the next best step.
Taking it one step further, AI can learn from large health data sets using deep learning and algorithms that analyze medical images, lab results, vitals, and charts.
Here are the core roles AI can play in your health system:
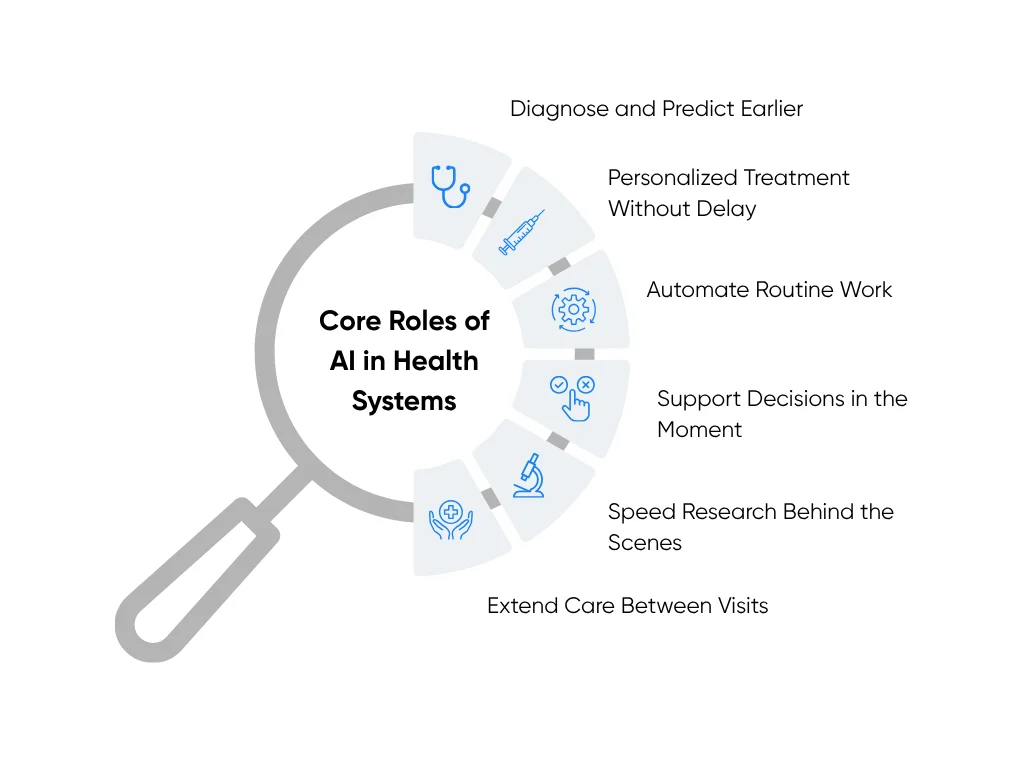
- Diagnose and predict earlier: That starts with imaging and signals from monitors. AI helps radiology flag tiny nodules or bleeds. It studies ECGs to spot early heart failure. It watches vitals for patterns that hint at trouble. Your team gets a heads-up while there is still time to act.
- Personalize treatment without slowing the clinic: AI compares each case with thousands of similar patients. It suggests options that fit the person in front of you. It ranks likely responses and side effects. You still decide. And you decide faster, with better context.
- Automate routine work so staff can breathe: Natural language processing tools draft encounter notes and capture structured fields. Scheduling tools fill gaps and reduce no-shows. Claims tools spot errors before submission. These small fixes add up across a week and across units.
- Support decisions in the moment: AI systems connect guidelines, labs, meds, and history in one view. They surface what matters for this patient, this visit. No hunting across tabs. No guessing which article still applies.
- Speed up research behind the scenes: Machine learning and big data systems screen millions of papers and data points. It narrows drug candidates and helps teams design smarter trials. That shortens the distance from idea to bedside.
- Extend care between visits: Remote monitoring and simple check-ins keep a steady eye on recovery. Wearables and connected devices feed data into models that spot risk early. Alerts go to the right person at the right time. Patients feel watched over without extra clinic trips.
These roles free up time, reduce delays, and make room for better patient conversations. To explore this further, we’ve put together a guide showing how hospitals use AI technology to simplify their daily operations.
Of course, every improvement comes with responsibility. AI must handle patient data with care and address potential privacy issues and ethical concerns from day one. That means:
- Protecting Privacy: Encrypt data, segment environments, and use strict access controls.
- Proving Safety: Validate models on your own population, then track drift and errors.
- Recording Every Action: Keep audit trails across data, prompts, outputs, and decisions.
- Keeping Humans in the Loop: Set clear review steps for high-risk tasks and overrides.
These guardrails protect trust while you scale. They also help you pass audits without pausing care.
You want results, not theater. We feel the same. At Aloa, we design pilots that fit your EHR and your staffing model. We start with one workflow and one metric. We measure impact in weeks, then expand what works.
As you weigh the pros and cons of AI in healthcare, keep this lens. AI’s role is to help your people act sooner, choose smarter, and spend more time with patients. When a tool does that, it earns its place. When it does not, you know what to do.
Pros and Benefits of AI in Healthcare
AI isn’t meant for replacing healthcare professionals; it’s making their work faster, more precise, and safer. It’s a powerful tool that can spot details people might overlook, handle repetitive tasks, and help teams focus on care instead of paperwork. When applied correctly, AI can strengthen every part of operations at a healthcare provider, delivering a clear return on your investment.
Here’s how those benefits play out across today’s hospitals and clinics:
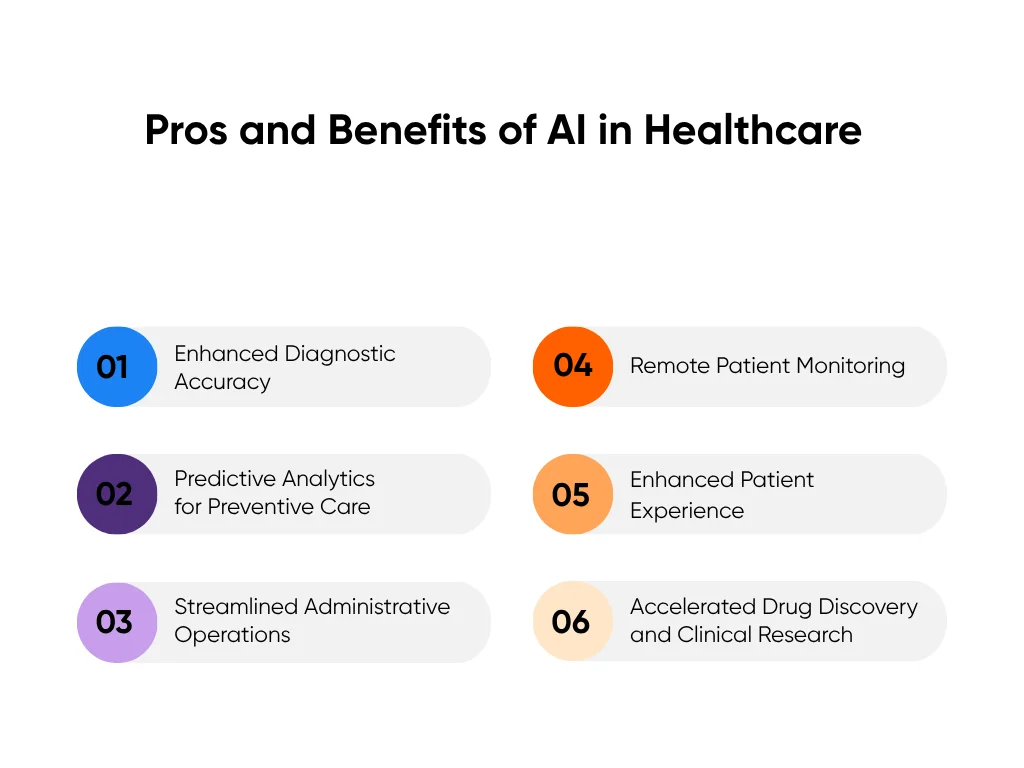
1. Enhanced Diagnostic Accuracy Through AI Imaging Analysis
AI imaging systems can now process scans like a seasoned radiologist. They analyze each pixel, compare findings against thousands of prior images, and highlight anything that looks unusual within seconds.
At Mayo Clinic, AI now detects subtle heart function changes from ECG data that standard tests miss. At Mass General Brigham, the Sybil model predicts lung cancer risk from a single CT scan with 94% accuracy, identifying early indicators months before symptoms appear.
Across specialties, the results are concrete:
- AI-assisted X-rays identify pneumonia, fractures, and tuberculosis with over 90% accuracy, cutting missed diagnoses by up to 20%.
- AI-driven MRI reconstruction shortens scan times by 40–50%, allowing hospitals to serve more patients daily.
- Pathology AI helps flag malignant cells and even grades tumor aggressiveness.
These systems give radiologists clearer data, reduce repeat scans, and improve patient outcomes. In hospitals using AI imaging, diagnostic accuracy and throughput often increase by 15–25% while error rates decline.
Aloa’s computer vision solutions are built for that kind of real-world performance: HIPAA-compliant, EHR-ready, and tested for clinical speed and accuracy.
2. Predictive Analytics for Preventive Care
Predictive analytics turns historical data into valuable insight. AI models can track patient vitals, labs, and trends to identify patterns before new symptoms appear. It helps clinicians and healthcare providers act before emergencies happen.
The use of Epic’s sepsis model was linked to a 44% lower chance of sepsis-related deaths among critical care patients. The Cleveland Clinic’s cardiac algorithm also detects early heart risks in cancer patients, prompting timely intervention. Systems like these have the potential to help reduce readmissions by 20-30% for chronic conditions such as heart failure, COPD, and diabetes.
The benefits extend beyond patients. Predictive analytics helps operations teams forecast ICU occupancy, improve resource allocation, anticipate staffing needs, and adjust supply orders. Health systems using predictive scheduling have reduced ER overcrowding and shortened wait times by 30%.
Preventing one unplanned readmission can save $9,000–$15,000 per patient. Across a mid-sized hospital, those savings easily scale into millions.
3. Streamlined Administrative Operations
Administrative tasks can eat up to one-third of a clinician’s time, often going towards transcribing visits, coding claims, filling scheduling gaps, and preventing billing errors.
Here are a few ways AI is already cutting through the admin clutter:
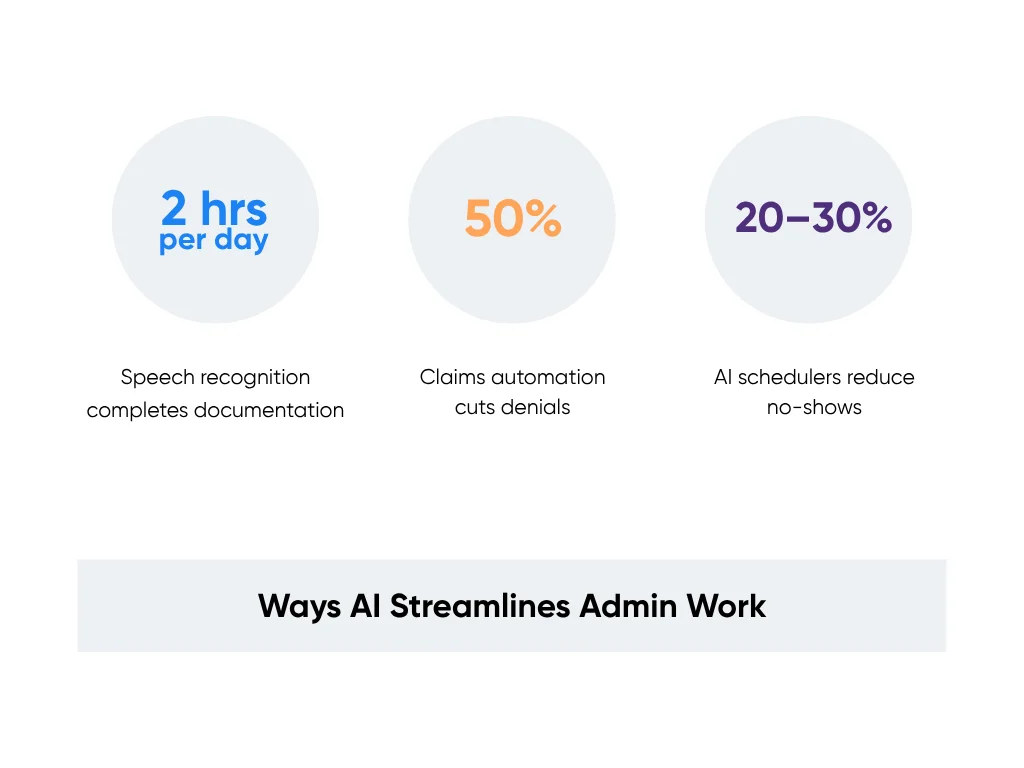
- Speech recognition tools complete documentation during visits, saving doctors an average of 2 hours per day.
- Claims automation systems cut denials by up to 50% and accelerate reimbursements.
- AI schedulers reduce no-shows by 20–30% by automatically filling cancellations.
Clinics using AI-based documentation have reported more patient-facing time and lower admin costs. That’s not just efficiency; it’s less burnout and smoother patient flow.
Aloa’s workflow automation systems are designed around your existing EHR, adding automation where it matters most without disrupting current operations.
4. Remote Patient Monitoring
Remote patient monitoring (RPM) extends care beyond the hospital. Smart devices track vitals such as glucose, heart rate, and oxygen levels and send continuous data to care teams. AI reviews the stream in real time, filters out false alarms, and alerts staff when patterns suggest trouble.
For example:
- A 2-pound overnight weight gain in a heart failure patient triggers an alert before fluid overload causes hospitalization.
- A spike in glucose levels in a diabetic patient prompts a call and treatment adjustment before complications arise.
Health systems using RPM have seen 30–50% fewer readmissions among high-risk patients and significant reductions in emergency visits. In chronic care management, RPM improves medication adherence and generates substantial cost savings through avoided hospitalizations and emergency care.
These tools also expand access for patients in remote or mobility-limited areas. Instead of another ER visit, a quick message keeps recovery on track.
5. Enhanced Patient Experience
AI improves the parts of healthcare patients notice most: communication, clarity, and convenience. It personalizes contact, answers routine questions instantly, and keeps patients engaged between visits. Here's how:
- AI chat assistants manage refills, reminders, and scheduling 24/7, freeing nurses for higher-touch care.
- Language translation tools simplify discharge instructions, which improves comprehension in non-English speakers.
- Predictive reminder systems reduce missed appointments while improving follow-up adherence.
At El Rio Health in Arizona, an AI appointment reminder system cut no-shows by 32%, recovering about $100,000 in monthly revenue and ensuring patients stay on schedule.
When patients understand their care and feel heard, adherence and outcomes rise. AI doesn’t replace empathy; it amplifies it by giving clinicians the time to connect.
6. Accelerated Drug Discovery and Clinical Research
AI is also transforming how new treatments reach patients. Instead of running every experiment manually, researchers use AI to model drug behavior, predict side effects, and identify viable compounds before lab testing begins.
AI screening reduces the time needed to identify drug candidates by up to 70%. In oncology research, medical AI has already uncovered new anticancer compounds in 8 months, a process that traditionally took 4–5 years.
Clinical trials benefit too. AI helps recruit the right participants, detect adverse events early, and ensure cleaner data. These improvements can cut trial costs while maintaining safety and reliability.
Hospitals using AI applications in medical research now complete studies faster and publish findings sooner. This brings effective treatments to patients years ahead of traditional timelines.
To cap it off, AI’s benefits in healthcare show up where they count most: data, patient outcomes, and staff well-being. It shortens diagnoses, prevents crises, reduces waste, and helps people stay healthier longer. But every advantage comes with tradeoffs. And understanding those risks is just as important as celebrating the wins.
Cons and Challenges of AI in Healthcare
AI has raised the bar for precision, speed, and efficiency in healthcare. But every leap forward brings its own set of challenges. The risks aren’t about whether AI belongs in healthcare, but how it’s built, tested, and used responsibly. These challenges don’t signal failure; they serve as checkpoints to ensure AI helps rather than harms.
1. Data Privacy and Security Risks
AI runs on some of the most sensitive information in healthcare, including medical records, charts, notes, and lab results. The same data that fuels better predictions can also expose healthcare systems to risk if it’s mishandled. According to the National Library of Medicine, data-sharing transparency remains one of AI’s biggest hurdles. Hospitals generate vast amounts of sensitive data every day, but inconsistent security practices and limited encryption controls leave gaps that attackers can exploit.
Every connected device, from EHR systems to wearables, creates a new entry point for breaches. In 2023 alone, over 133 million patient records in the United States were affected by healthcare data breaches. Each leak can lead to regulatory fines, damaged trust, and real harm to patients.
Healthcare data is especially attractive because it’s permanent; you can’t “reset” your medical history like a password. And as AI models train on large datasets, the need for secure, anonymized, and traceable data grows.
To manage this data security risk, organizations are turning to federated learning, a method that trains AI models across decentralized data without sharing the raw files. Paired with end-to-end encryption and strict access controls, it’s one of the most effective ways to protect patient privacy while still improving model accuracy.
Aloa also helps healthcare teams design HIPAA-compliant systems that keep health data private without slowing innovation. Our approach ensures encryption, logging, and monitoring are built into every workflow.
2. Resistance to Adoption
In healthcare, hesitation isn’t fear. It’s due diligence. Clinicians have every reason to be cautious. When lives depend on accurate diagnoses, the cost of a wrong algorithmic call is too high to gamble on. Many providers are reluctant to rely on tools they don’t fully understand or can’t easily validate.
Resistance often stems from three things: lack of trust, workflow disruption, and unclear accountability. If an AI recommendation conflicts with a clinician’s judgment, who’s responsible for the outcome? That uncertainty slows adoption.
But resistance isn’t a dead end; it’s a filter. It forces developers to build AI systems that are transparent, explainable, and integrated into existing routines. When AI fits into a clinician’s workflow instead of forcing new habits, acceptance rises.
Hospitals that pair training with pilot programs see faster, more confident implementation. Departments that co-develop AI tools with their clinical staff, rather than pushing systems top-down, build trust early and see smoother transitions into daily use.
For leaders looking at practical ways to align AI with everyday medical decision-making, our guide on applying AI responsibly in clinical settings covers what works and what doesn’t.
3. Data Availability and Accessibility
AI learns from data, but healthcare data isn’t always ready to teach. It’s often trapped in outdated systems, fragmented across departments, or formatted inconsistently. And poor data quality (missing, mislabeled, or incomplete) can distort AI predictions and amplify bias.
Small or rural hospitals face another issue: limited data volume. Their patient populations may not represent the diversity AI systems need to perform reliably. If models are trained mainly on urban or academic datasets, they risk underperforming in community settings.
Solving this requires a focus on data standardization and interoperability. Shared frameworks like FHIR (Fast Healthcare Interoperability Resources) help unify health records across platforms. With better integration, AI models can learn from larger, more representative datasets.
AI’s promise depends on access, not abundance. Systems that can safely connect and share insights across facilities, not just hoard data, will see the most accurate outcomes.
4. Limited Examples of AI Integration
Despite hundreds of AI healthcare pilots, only a fraction scale to full deployment. Many systems stall after the prototype stage because they can’t integrate smoothly into EHRs or meet strict compliance demands. The Narrative Review notes that only a small percentage of AI models validated in labs ever reach live clinical use.
Integration challenges usually come down to three gaps: technical compatibility, clinical validation, and maintenance. Models built in isolation often fail to align with real hospital data or workflows. Even when they work well in theory, ongoing updates, retraining, and regulatory audits require long-term resources most teams aren’t staffed for.
To close this gap, healthcare organizations are adopting modular AI solutions: smaller, workflow-specific tools instead of large, all-encompassing platforms. These can plug into existing systems without major rebuilds.
At Aloa, we specialize in scaling pilot models into production-ready tools. Our AI integration services focus on making solutions operational, secure, and sustainable over time.
5. High Costs of Development
AI isn’t cheap. Developing models, testing them under HIPAA compliance, and maintaining secure infrastructure can cost millions. Training data alone often needs cleaning, labeling, and validation, all of which require human expertise.
Legacy systems make it much more challenging as well. Many hospitals still run on older EHR software, meaning new AI tools need costly middleware or manual integration. Add regulatory audits, cybersecurity insurance, and model retraining, and the total investment rises quickly.
But the cost equation is changing. AI-assisted software development now speeds up the build process itself. Using tools like automated code generation and machine learning model templates, developers can prototype new healthcare solutions in weeks instead of months. Long-term savings come from faster iteration and fewer post-launch fixes.

The key is to start small: target a single workflow or clinical practice, validate results, and scale from there. Hospitals that use this approach often see ROI within 6 to 12 months, especially when focusing on high-value areas like documentation or imaging.
AI will always test the limits of what healthcare can do. The trick is keeping progress steady while staying grounded in patient safety and practical execution. And that’s exactly where the right development partner makes all the difference, one that understands both the tech and the realities of care.
Build Your AI Healthcare Software with Aloa
We work alongside doctors, researchers, and healthcare innovation leads, building real AI tools that fit clinical reality, not just lab conditions. From imaging and diagnostics to workflow automation and predictive analytics, our teams focus on software that’s HIPAA-compliant, explainable, and tested under real pressure.
Our ongoing projects range from AI transcription tools that reduce reporting time to secure computer vision systems for faster, more accurate diagnostics. We handle the full healthcare AI development process, from concept to development, compliance, and deployment.
Pricing is simple; no hidden costs, no retainers. You can view clear, transparent rates for every project size on our AI pricing page.
With Aloa, you’re getting a partner that builds AI that works on the floor, in the clinic, and for the people delivering care every day.
Key Takeaways
The pros and cons of AI in healthcare shape the real decisions leaders like you make. AI is changing how care gets delivered, but it still starts with people who want faster answers, safer systems, and a little breathing room in the day.
And the biggest wins don’t come from replacing what already works. They come from using tech to make the work lighter, clearer, and more consistent. The risks? They’re real, but manageable when you move with purpose, rely on clean data, and partner with people who know what real clinical pressure feels like.
If you’re exploring what AI could do for your team, reach out to us. Tell us what’s getting in your way, and we’ll help you figure out the next smart step.
You can also join us on Discord or subscribe to our newsletter to swap ideas with other healthcare innovators building the next generation of safe, practical AI tools.
FAQs
1. How can AI help reduce healthcare costs?
AI cuts costs by doing the work that slows your team down: automating billing, scheduling, and documentation, reducing diagnostic errors, and predicting patient risks before they become emergencies. Hospitals using AI for operations often see 20–30% lower administrative costs and faster throughput without adding staff.
2. Can AI help with staffing shortages and burnout?
Yes. AI takes repetitive work off clinicians’ plates, like drafting notes, managing forms, and handling routine patient inquiries. That means less time typing and more time with patients. When teams use tools that lighten the load, burnout drops and job satisfaction rises.
3. How do I keep AI solutions HIPAA-compliant?
Start with vendors who build for compliance, not around it. Look for HIPAA-compliant systems with encryption, access controls, and full audit trails. Aloa designs healthcare AI with compliance built in from day one; see how in our guide on making any AI model HIPAA-safe.
4. How do I handle staff resistance to AI?
Keep it open and collaborative. Most pushback comes from uncertainty, not opposition. Involve staff early, show quick wins, and make it clear AI is here to assist, not replace. When people see that AI gives them time back, skepticism turns into buy-in.
5. How much does AI implementation cost?
It depends on your goals. Smaller automation tools can start at a few thousand dollars a year, while enterprise-level systems can reach six figures. The key is ROI. Most hospitals recover costs within 12–24 months through efficiency gains and fewer errors.
6. What should I look for in an AI development partner?
Choose a team that understands both the tech and the pressure of care. Look for proven healthcare experience, HIPAA and FDA knowledge, transparent workflows, and long-term support. Aloa connects you with vetted AI developers who specialize in building tools that perform safely, securely, and under real clinical conditions.

