Doctors spend almost half their day using electronic health records instead of caring for patients, or two hours documenting for every hour of care. You need a way to ease that burden without disrupting care.
AI EMR data processing helps you do that. It reads notes, identifies key details, and automatically fills in records. It uses natural language processing to understand text and machine learning to sort and check information. You get faster charting, better data quality, and fewer mistakes to fix later.
At Aloa, we build AI systems that connect with your existing EMR tools. We focus on privacy, security, and smooth rollouts, so your team saves time while your systems stay safe and compliant.
This guide shows you:
- How AI EMR data processing handles structured and unstructured data
- What tech and compliance prep you need
- How to assess vendors and plan a pilot
- Integration patterns for FHIR, HL7, Epic, and Cerner
- Realistic timelines, budgets, and KPIs
- How to get clinicians on board and prove real value
You’ll leave with a clear plan to make AI work in your organization: safe, practical, and ready to scale.
TL;DR
- AI EMR data processing turns raw electronic records into structured, usable data through natural language processing and machine learning.
- Doctors spend nearly half their day in EHR systems; automation can cut documentation time by up to 30%.
- AI organizes structured, semi-structured, and unstructured data, improving accuracy and reducing manual data entry.
- Strong infrastructure (hardware, secure APIs, and stable networks) forms the base for reliable implementation.
- Compliance with HIPAA and HITECH is essential before live deployment; encrypt and audit all patient information.
- Vendor selection should prioritize healthcare experience, performance metrics, and continuous model retraining.
- Implementation follows five key stages: planning, setup, migration, testing, and rollout.
- Testing includes functional, compliance, and user acceptance reviews to validate performance and patient safety.
- Gradual rollout and clinician trust ensure adoption and measurable ROI.
How Does AI EMR Data Processing Technology Work?
AI EMR data processing uses natural language processing to read free-text notes, automates data entry, and applies machine learning to find patterns in patient records and medical history. It turns raw clinical data into structured information you can use immediately to speed documentation, reduce mistakes, and guide better clinical decisions.
Every EMR holds three main types of medical data:
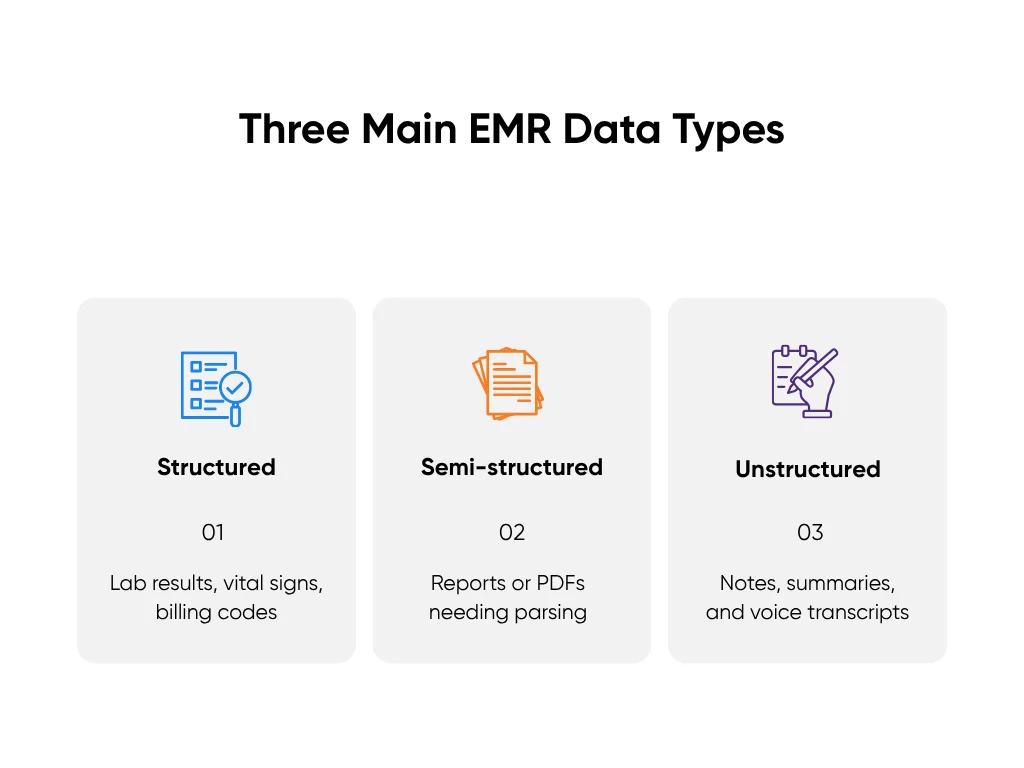
- Structured: Numbers and codes already in set fields, like lab results, vital signs, and billing codes.
- Semi-structured: Reports or PDFs with headers or sections that still need parsing before they become searchable.
- Unstructured: Notes, discharge summaries, and voice transcripts that hold key insights but sit buried in text.
AI systems process these layers differently to provide clinical decision support. Structured data connects straight to dashboards and reporting tools. Semi-structured data passes through extraction models that recognize text, dates, and measurements inside images or scanned files. Unstructured data runs through natural language processing, which reads language like a clinician would, identifies medical terms, and maps them to categories like diagnoses, symptoms, or medications.
Once the system organizes the data, machine learning checks it for accuracy and meaning. It flags inconsistencies, predicts missing values, and finds correlations, such as lab trends signaling risk or duplicated orders driving higher costs. With each record processed, the model sharpens its accuracy and speed.
Researchers have found that AI can read doctors’ notes accurately and pull out key details, which helps teams review data and run studies much faster.
In practice, this means your teams spend less time typing and correcting and more time on clinical care and patient engagement. Charting is faster. Reporting is instant. Clinicians view clear summaries instead of endless notes. You finally see your EMR as a working tool, not a digital filing cabinet.
See our guide for a broader view of ops impact across scheduling, documentation, and revenue. From here, success depends on preparation: understanding your infrastructure, compliance needs, and rollout plan. That's where we head next.
Planning and Requirement Assessment for an AI EMR Data Process Tool
Before you roll out any AI system, you need to know if your setup can take the load. AI EMR data processing doesn’t fix a weak foundation; it amplifies it. If your infrastructure is shaky or your compliance policies are half-built, your results will be too. This step is where AI projects earn credibility or collapse under their own weight.
Technical Infrastructure Assessment
Think of this as your system stress test. AI systems move large volumes of data across multiple layers (databases, APIs, analytics dashboards), and they don’t wait around for slow servers. You need hardware that can handle large data sets and load spikes, software that integrates cleanly, and a network that stays fast under pressure.
Here’s the short version:
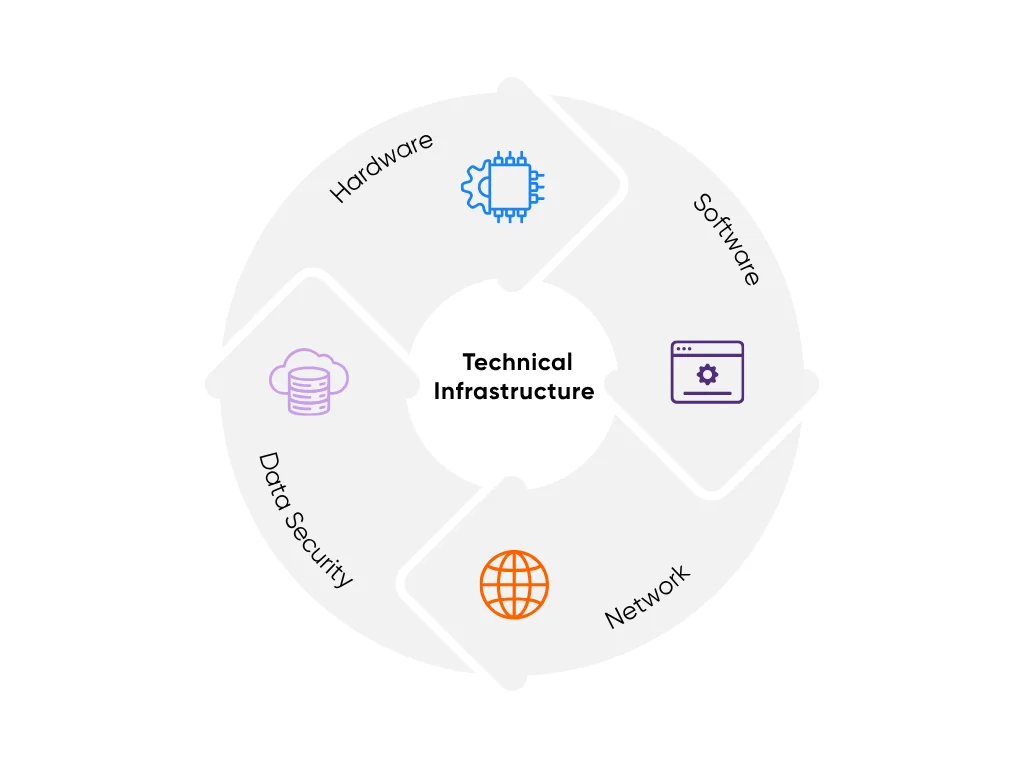
- Hardware: For a pilot, start with 16 vCPUs, 64 GB RAM, and SSD storage. For long-term scaling, multiply that footprint by your daily encounter volume. On-prem or cloud doesn’t matter as long as it meets HIPAA and HITECH security standards.
- Software: Confirm your EMR supports modern integration of AI. Epic and Cerner handle FHIR 4.0 and HL7 feeds, but older versions may throttle performance or block data access. Test endpoints early using dummy records before you spend a dollar on modeling.
- Network: Keep latency below 50 milliseconds between your AI layer and EMR database. Anything slower and clinicians will notice. Independent studies link heavy EHR time to higher burnout. Stability beats speed; predictable response times build trust.
- Data Security: Use encryption across every layer and maintain role-based access. Audit logs must track every connection, model run, and data pull.
You want the infrastructure to feel invisible. When it’s solid, AI becomes part of the workflow. When it’s not, you’ll hear about it by the second chart.
For a non-technical primer you can share with leadership, here’s a practical playbook for decision-makers.
Regulatory and Compliance Preparation
HIPAA defines how patient data moves, HITECH sets penalties for breaches, and your internal governance policies decide who can touch what. Start there. Have your AI vendor sign a Business Associate Agreement (BAA) before they see a single record.
Keep this short checklist handy:
- Encrypt all PHI, both in transit and at rest
- Limit access to essential roles only
- Test every FHIR/HL7 endpoint in a sandbox before live use
- Record every model interaction for audit purposes
Organizational Change Management
Technology often is the “easy” part. It won’t work without change management, training, and a cohesive set of processes. Assign clear owners for every area (clinical, data, and IT). Run your pilot in the background, quietly learning and predicting, while your team manually compares results.
Hospitals using AI tools to help with notes report about a 30% drop in documentation time and less burnout among clinicians. When clinicians see fewer clicks and faster notes, you’ll earn adoption without asking for it.
Once your infrastructure, compliance, and team are ready, the next step is vendor selection: choosing a partner who understands your systems, your data, and your pace.
How to Evaluate and Find the Right Vendor?
The partner you choose will decide how far your AI project goes. Some vendors sound impressive but don’t understand healthcare. The best ones know how hospitals work: how data flows, how privacy rules apply, and how to make tools that fit into a clinician’s day instead of slowing them down
Vendor Capability Assessment
The right vendor needs three things: experience, performance, and trust.

1. Real Healthcare Experience
Avoid vendors who build “AI for everything.” You need a team that’s already worked with EMR systems like Epic, Cerner, or OpenEMR. Ask for examples of projects that handled protected health information under HIPAA. They should be able to describe which workflows they’ve automated and what results they achieved. If they can’t, that’s a red flag.
You can also look at our HIPAA-compliant medical transcription project for a concrete example of secure, audited workflows.
2. Proven Performance
Skip vague promises and ask for proof. A good vendor can show you clear benchmarks:
- Data extraction accuracy above 90%
- Query speed under one second
- System uptime above 99.9%
- Evidence of bias testing and validation reports
- Working integrations with FHIR 4.0 and HL7
Ask to see a mock data run across de-identified data sets that mirror your treatment plans and coding rules. A vendor that truly understands healthcare will show working examples, not PowerPoint slides.
3. Reliable Support
AI isn’t a one-and-done install. You need a partner that retrains models as data changes, maintains uptime, and keeps audit logs for every transaction. Look for regular updates, 24/7 monitoring, and retraining plans built into the contract.
At Aloa, we’ve done this with mid-sized health systems running Epic and Cerner. We design for compliance first, speed second, and reliability always.
Pilot Program Design
A pilot keeps the stakes small but the learning big. It tests whether the AI fits your real workflows and data.
Try this simple structure:
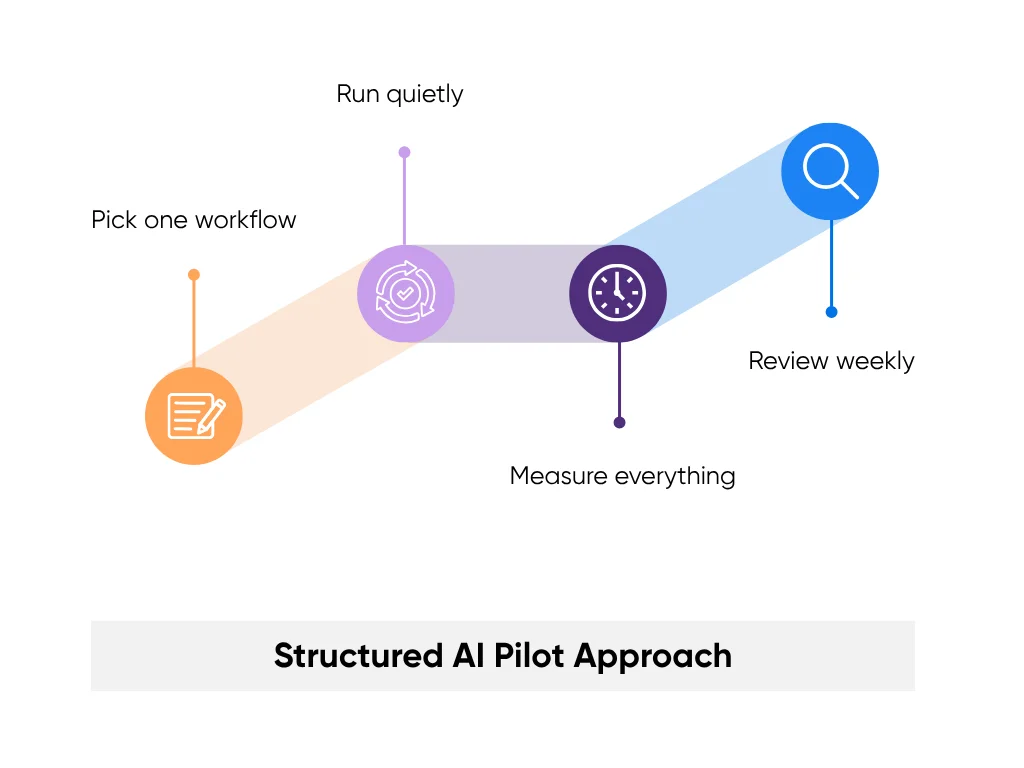
- Pick one workflow: Start small, like automating discharge summaries or summarizing physician notes.
- Run quietly: Let the AI process live data in “shadow mode” without changing anything in production.
- Measure everything: Time saved, accuracy rate, privacy incidents. Keep it simple and specific.
- Review weekly: Adjust, retest, repeat. A good vendor will pivot with you instead of pushing canned updates.
A strong pilot proves what works before scaling. It turns talk into evidence.
Contract and Partnership Considerations
Once the pilot delivers, focus on the agreement. It defines who owns what and how accountability works. Your contract should include:
- A BAA before data access
- Ownership terms for your data and AI outputs
- Service levels (SLAs) for uptime, latency, and accuracy
- Audit rights for logs, model updates, and reports
- An exit plan so you can leave without losing your data
Contracts protect both sides, but real partnership runs on transparency. Your vendor should explain technical details in plain terms and answer every compliance question without jargon.
At Aloa, we treat every build like a shared project. We explain our process, show our results, and stay connected after launch. You can see more of how we work on our YouTube channel.
When that trust with your vendor is in place, you’re ready to scale from pilot to production. Let’s look at how to plan that rollout.
Step-by-Step Implementation Process
Implementing AI EMR data processing is most effective when rolled out incrementally. The aim is to make the tool part of daily work.
Implementation Phases and Timelines
AI projects move best in five stages:
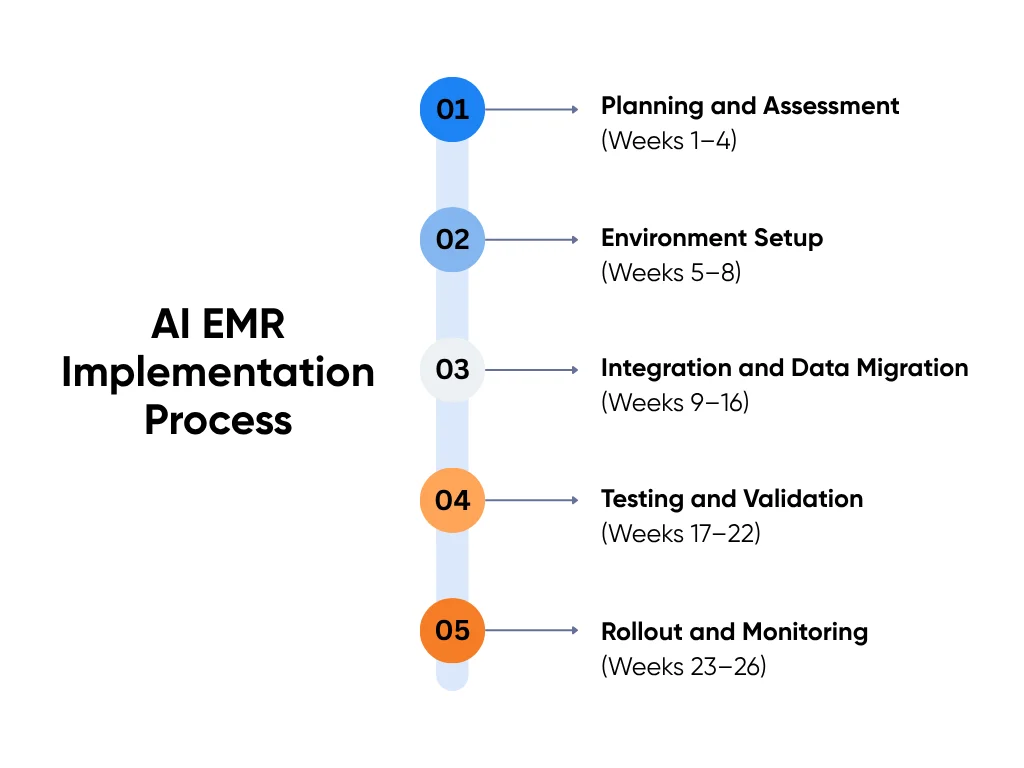
1. Planning and Assessment (Weeks 1–4)
Map where AI helps most (if you need ideas, browse real-world AI use cases that deliver value). Pick high-friction tasks like manual data entry or coding. Define scope, success metrics, and owners in data, IT, and compliance. End this phase with a signed plan, budget, and timeline.
2. Environment Setup (Weeks 5–8)
Build safely in a test space that mirrors your EMR. Configure secure APIs and access controls. Use synthetic data to confirm the setup. Finish with a working sandbox ready for pilot data.
3. Integration and Data Migration (Weeks 9–16)
Connect the AI to your EMR. Map fields such as diagnoses, medications, vitals, and treatment history. Migrate recent records first. Run small, staged imports. A clean first sync confirms your mappings and data flow.
4. Testing and Validation (Weeks 17–22)
Run in shadow mode. The AI reads and structures data without changing live records. Compare results to human output to check accuracy, speed, and privacy. When accuracy stays above 90% and security checks pass, you're ready for live use.
5. Rollout and Monitoring (Weeks 23–26)
Go live by department. Track performance, error rates, patient satisfaction trends, and clinician usage on a dashboard. If everything stays stable for 30 days, expand to more units. Success looks quiet and reliable.
Data Migration and Integration
AI systems must read and write data safely. Build a controlled bridge between your EMR and the AI layer.
Use FHIR 4.0 or HL7 interfaces. Follow this checklist:
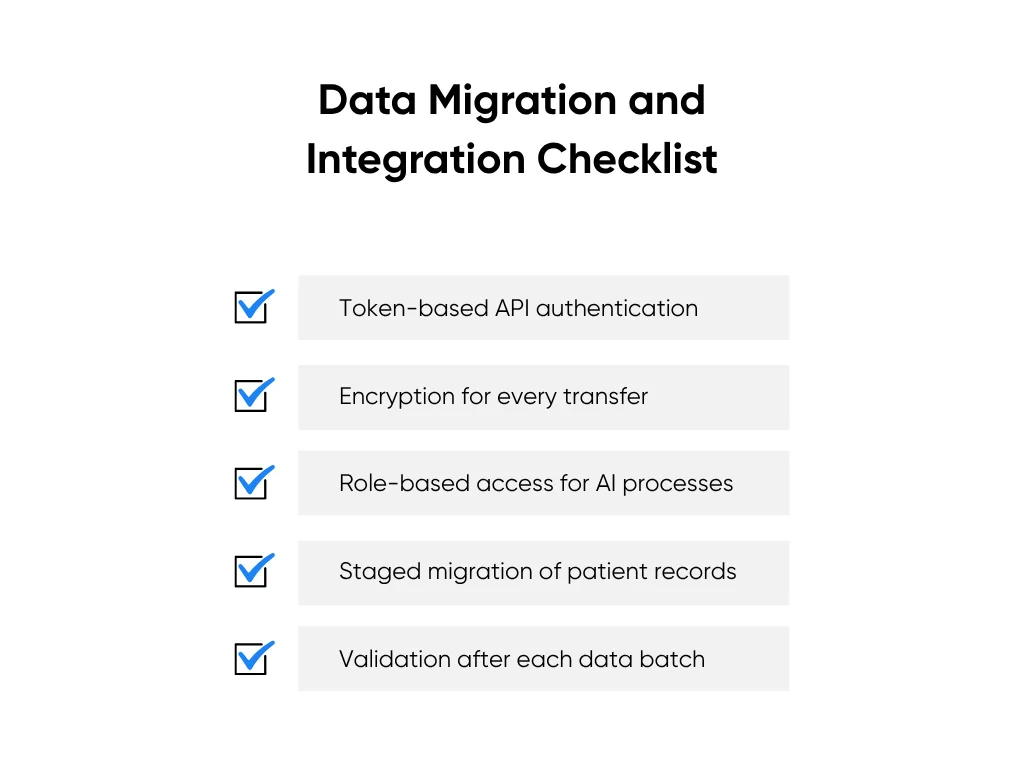
- Token-based API authentication
- Encryption for every transfer
- Role-based access for AI processes
- Staged migration of patient records
- Validation after each data batch
Keep older records separate during the pilot. After stability is proven, bring legacy data over in batches to avoid slowdowns and duplicates.
We created a short guide on building HIPAA-safe AI systems if you’d like a deeper look at how to keep your models secure and compliant.
Testing and Validation Protocols
Testing turns a demo into a dependable system. Cover three layers:
- Functional Testing: Confirm the AI captures, labels, and updates the right fields.
- Compliance Testing: Verify HIPAA and HITECH controls. Check encryption, permissions, and audit logs.
- User Acceptance Testing: Let healthcare professionals use the tool in real clinical workflows. Collect feedback, fix gaps, and retest.
You are ready to scale when clinicians trust the results and compliance has approved every data flow. From there, focus on tracking time saved, error reduction, and throughput so the ROI is clear.
Key Takeaways
AI EMR data processing only works when it gives time back to clinicians and helps your systems keep up with daily care. Start with what causes the most frustration. Pick one process that slows your team down and fix that first. Build a strong base, test everything, and move forward only when your data is clean and compliance is in place. That’s how real progress lasts.
The teams seeing success didn’t rush. They took it step by step, kept data secure, and built trust through small wins that added up. If you’re ready to do the same, we’d love to help you get there.
Start a conversation with us and share what you’re working on. You can also connect with our AI Builder Community on Discord or get simple, useful tips from our newsletter.
FAQs About AI EMR
1. What is AI EMR data processing, and how is it different from a regular EMR?
AI EMR uses tools like natural language processing and machine learning to read, organize, and analyze medical records automatically. Unlike traditional EMRs that only store data, AI systems clean up unstructured notes, find patterns, and pull out key details. This reduces manual work, improves accuracy, and helps healthcare providers make faster, better decisions.
2. How long does it take to set up AI EMR data processing?
Most healthcare organizations take 3 to 9 months to go live, depending on scope and big data needs. Smaller clinics move faster, while large hospitals need more time to handle complex systems and multiple sites. A good rollout usually includes:
- Planning and assessment (about 4–6 weeks)
- Setting up infrastructure and choosing a vendor (6–8 weeks)
- Running a pilot (8–12 weeks)
- Data migration and testing (8–12 weeks)
Starting small, like one department, helps keep timelines realistic.
3. How much does AI EMR data processing cost?
Costs depend on your size and setup. Small practices often spend $50,000–$150,000 in the first year, while large networks might invest $500,000–$2 million. Common expenses include software licenses, setup and integration, data migration, staff training, and maintenance. Most teams see a return within 12–24 months through faster documentation, better coding, and lower admin costs.
4. Is AI EMR data processing HIPAA compliant?
Yes, when done right. Pick a vendor that signs a BAA, encrypts all data, uses secure servers, and keeps full audit logs to protect patient information. Your IT team should check that the AI runs in a HIPAA-compliant environment, uses role-based access, and follows strict data governance policies. At Aloa, we design every healthcare AI system to meet these standards from day one, so your team can focus on patient care. Always review these safeguards with your compliance officer before going live.

