In healthcare, seamless integration is crucial for efficient EMR API integration, ensuring a strategic build and deployment approach. Businesses and startups are often challenged to integrate electronic medical records (EMR), patient data, and clinical information into cohesive systems.
Aloa understands the importance of patient records, medical devices, and data exchange in healthcare. The strategic approach to EMR integration with API involves addressing key aspects such as regulatory compliance and interoperability and integrating crucial components like patient outcomes and medical billing. Aloa comprehensively guides you on building and deploying an EMR API integration, catering to digital health startups and established healthcare providers' needs.
This blog delves into the process of building and deploying EMR API integration, best practices and its core features. Afterward, you will gain a profound understanding of the strategic build and deployment of EMR integration with API, empowering them to streamline workflows, reduce costs, and enhance healthcare delivery.
Let's dive in!
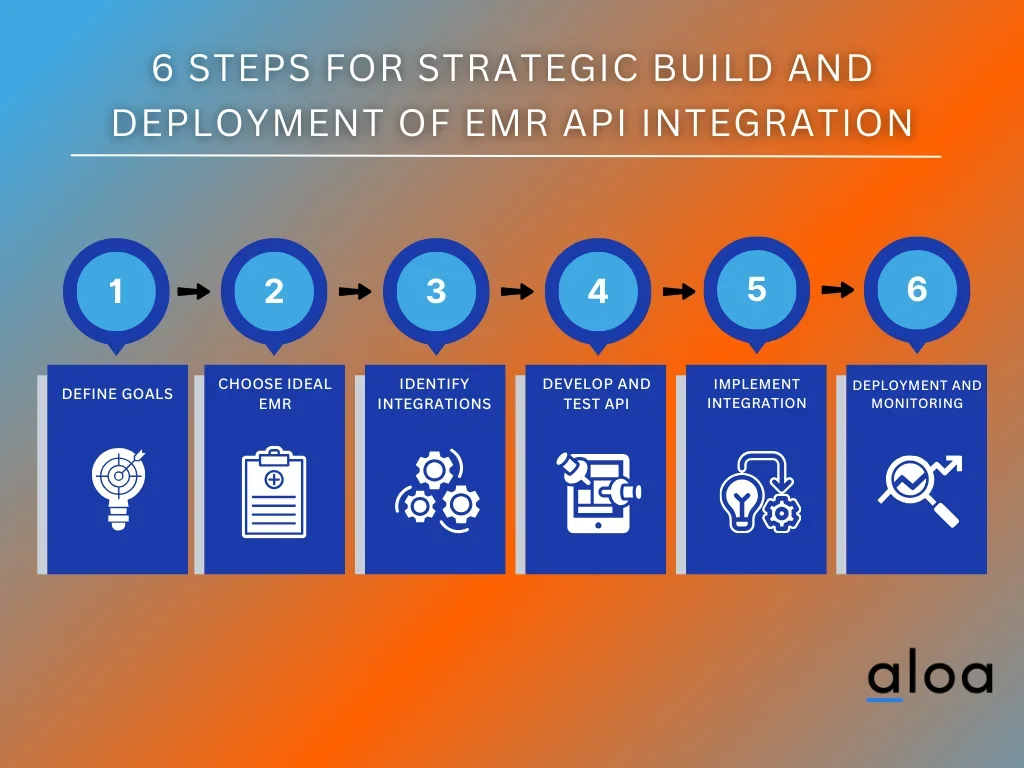
6 Steps for Strategic Build and Deployment of EMR API Integration
Strategically building and deploying an EMR API integration requires a systematic approach to ensure seamless functionality within healthcare systems. These six essential steps are a blueprint for success, encompassing meticulous planning, development, and implementation from initial assessment and requirement gathering to testing, integration, and ongoing maintenance.
Here are six steps for strategically building and deploying EMR API integration:
Step 1: Define Objectives and Scope
Defining clear objectives and scope is the foundational step in any EMR API integration project. This initial phase sets the direction for the entire endeavor, ensuring alignment with overarching goals and priorities. Here are the things to consider:

- Patient Data Access: Determine how improved access to clinical data through integration can enhance patient experience and care quality.
- Data Entry Reduction: Identify areas where integration can minimize data entry errors, critical for accurate patient documentation and care.
- Interoperability Enhancement: Assess the potential benefits of enhanced interoperability with other healthcare systems, such as practice management tools, telehealth platforms, or analytics applications.
- Administrative Streamlining: Explore opportunities to streamline administrative tasks like appointment scheduling, billing, and paperwork through integration.
- Scope Clarity: Clearly outline the boundaries of the integration project, specifying which EMR systems are involved, what patient information will be shared, and what desired outcomes are expected.
By carefully considering these aspects, healthcare organizations can chart a strategic course for their EMR integration with API, optimizing patient care, reducing operational burdens, and fostering stakeholder collaboration. This crucial step ensures that the integration efforts align with the healthcare institution's broader goals while considering regulatory compliance and data security concerns.
Step 2: Select the Right EMR System
Selecting the right Electronic Medical Records (EMR) system is a pivotal step in the process of EMR API integration, as it lays the foundation for seamless data exchange and interoperability. Here are some considerations to expand on this step:
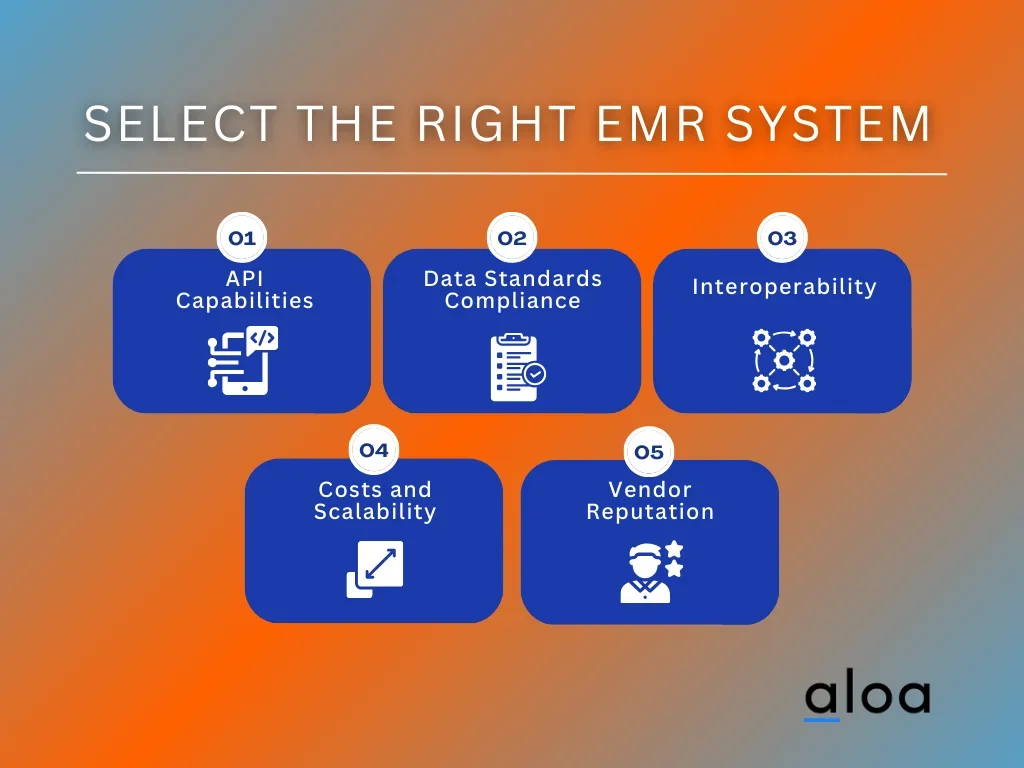
- API Capabilities: When choosing an EMR system, prioritize those that offer robust and modern API capabilities. Not all EMR systems are created equal in this regard. A well-designed API allows efficient and secure communication between the EMR system and other healthcare applications, such as telemedicine platforms or AI-driven tools.
- Data Standards Compliance: Look for an EMR system that complies with healthcare data standards like HL7 FHIR. This compliance simplifies data exchange and ensures that health data, including patient test results and medical history, can be easily shared and interpreted across different systems.
- Interoperability: Consider the level of interoperability the EMR system offers. An integrated EHR (Electronic Health Record) is crucial for healthcare providers to access a patient's complete medical history and make informed decisions. Verify if the EMR system can seamlessly integrate with other EHR systems and applications.
- Costs and Scalability: Evaluate the cost of implementing and maintaining the EMR system. Consider your organization's budget and scalability needs. High costs can be a barrier to entry, so balancing functionality and affordability is essential.
- Vendor Reputation: Research the reputation of the EMR system vendor within the healthcare industry. Renowned vendors like Epic often have well-established systems and extensive support resources.
Selecting the right EMR system with strong API capabilities and compliance with data standards is fundamental to a successful EMR integration with an API project. It ensures that health data can flow smoothly, enabling healthcare providers to leverage the power of modern technologies and applications to enhance patient care.
Step 3: Identify Integration Needs
It is imperative to conduct a thorough evaluation of the specific integration requirements. This involves meticulously scrutinizing the types of data that must flow between the EMR system and other interconnected healthcare systems or applications. Data elements may encompass a broad spectrum, including but not limited to patient demographics, medical history, laboratory results, appointment scheduling, and more.
Prioritization is a pivotal aspect of this step. It involves assessing the integration needs through their impact on patient care and operational efficiency. Some data elements, such as immediate access to critical medical records or lab results, may significantly affect patient outcomes. In contrast, others may primarily influence the administrative aspects of healthcare delivery.
By establishing clear priorities, healthcare organizations can allocate resources efficiently, focusing on the integrations that will yield the most substantial benefits regarding patient well-being and streamlined operations. This strategic approach ensures that integration efforts are directed toward the most pressing and valuable areas, optimizing the overall impact on healthcare delivery.
Step 4: Develop and Test API
Developing and testing APIs is a critical phase in the strategic build and deployment of EMR API integration, demanding meticulous attention to detail and adherence to best practices. Here's an expanded view of this step with crucial considerations:
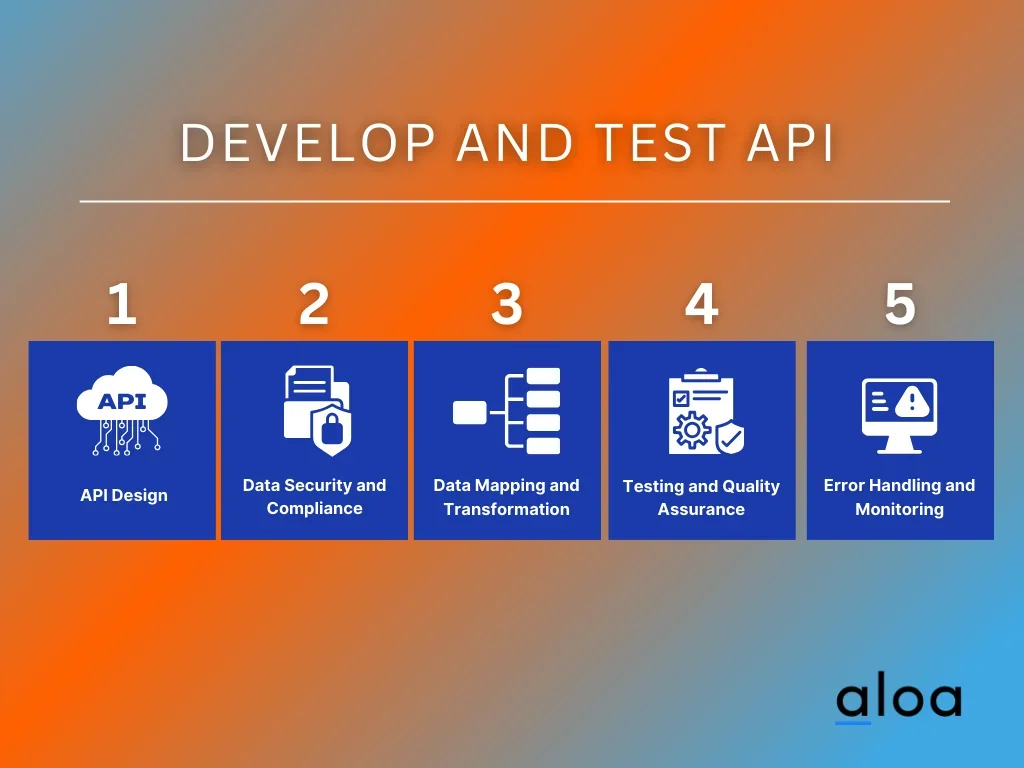
- API Design: Develop APIs that serve as a bridge between your EMR system and other healthcare applications. Focus on creating RESTful or SOAP APIs that facilitate seamless communication. Consider using modern healthcare data standards like HL7 FHIR for improved interoperability.
- Data Security and Compliance: Ensure that data transmitted through the APIs is encrypted using robust encryption protocols (e.g., TLS/SSL) to safeguard patient information. Comply with healthcare data privacy regulations, such as HIPAA (Health Insurance Portability and Accountability Act) in the United States, to protect patient confidentiality. Implement robust authentication and authorization mechanisms to restrict access to authorized users.
- Data Mapping and Transformation: Pay close attention to data mapping and transformation during API development. Ensure that data from the EMR system is structured correctly and standardized for accurate exchange with other systems. Handle data discrepancies and variations effectively to maintain data integrity.
- Testing and Quality Assurance: Rigorously test the APIs in a controlled environment to uncover potential issues. Conduct unit, integration, and end-to-end testing to verify data accuracy, performance, and security. Use testing tools and methodologies to simulate real-world scenarios and ensure the APIs can handle varying loads.
- Error Handling and Monitoring: Implement robust error-handling mechanisms within the APIs to manage unexpected situations gracefully. Establish monitoring and logging systems to track API performance and detect real-time anomalies. Set up alerts to promptly address issues that may arise during data exchange.
Developing and testing APIs is foundational to the success of EMR integration with API, ensuring that patient data flows securely and accurately between systems. Thorough testing and compliance measures help create a robust, reliable integration that enhances healthcare delivery and patient care while safeguarding sensitive information.
Step 5: Implement Integration
Implementing integration solutions within healthcare software demands meticulous planning and execution. Here's how to navigate this critical phase:
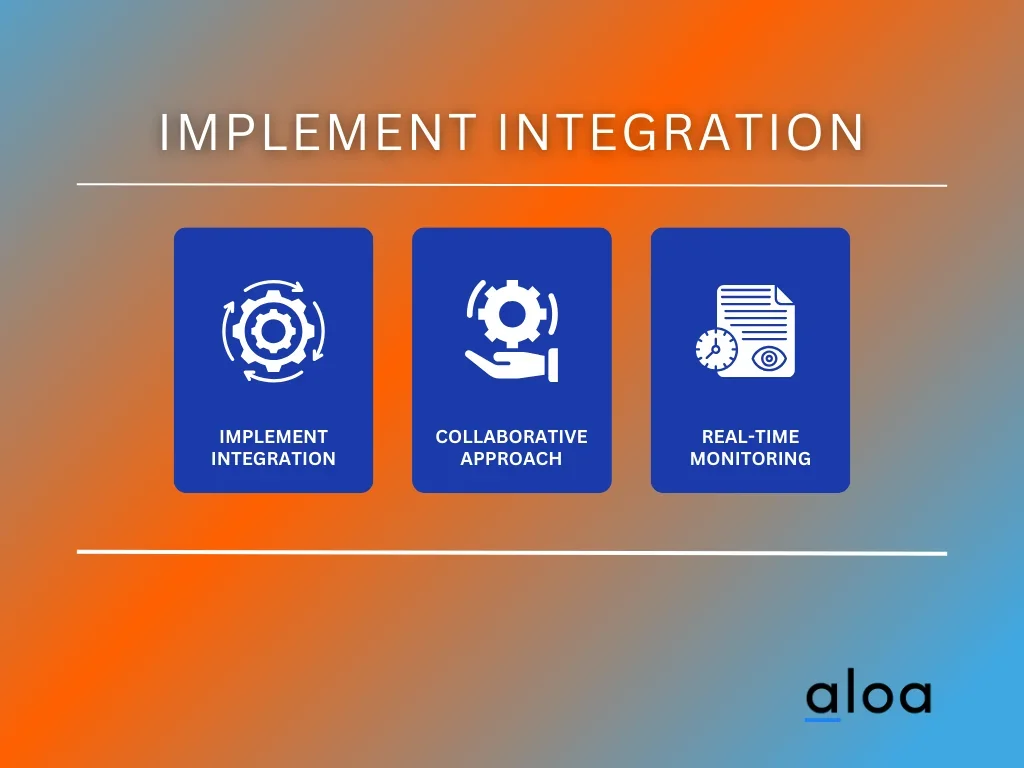
- Controlled Deployment: Initiate the integration in a controlled setting, like a test or staging environment. This pre-rollout phase allows for comprehensive testing without affecting the live production environment, mitigating potential risks.
- Collaborative Approach: Forge strong collaboration among EMR vendors, IT teams, and healthcare professionals. Their collective expertise ensures a comprehensive understanding of the integration's impact and facilitates a smoother deployment process.
- Real-time Monitoring: Monitor the integration's performance in real-time post-deployment. Establish proactive mechanisms to address any issues that arise swiftly. Continuous monitoring ensures prompt troubleshooting, minimizing disruptions in patient care or operational workflows.
Implementing integrations requires careful orchestration and a commitment to ongoing refinement. This approach ensures seamless integration between software components, fostering interoperability and optimizing the software's functionality within the healthcare ecosystem.
Step 6: Deployment and Monitoring
Deployment and monitoring are critical in integrating software solutions within the healthcare industry. To ensure a smooth transition, deployment is executed in a controlled and staged manner, minimizing disruptions to daily healthcare operations. This staged approach involves careful testing in controlled environments before a full-scale rollout, allowing for the identification and resolution of potential issues proactively.
Once deployed, continuous monitoring becomes imperative. Performance, data integrity, and security are closely scrutinized. Implementing robust alerting and monitoring systems ensures the swift detection and response to any anomalies or issues that may arise. This real-time vigilance is instrumental in maintaining the seamless operation of integrated systems, safeguarding patient data, and preserving the overall integrity of healthcare processes.
In tandem with monitoring, a well-defined maintenance plan is established. This plan addresses updates, upgrades, and changes in EMR systems or external components that might impact the integration. By proactively managing these changes, healthcare organizations can stay ahead of potential challenges, ensuring the continued efficiency and reliability of integrated software solutions in the healthcare industry.
Core Features of EMR API Integration
EMR API integration, an essential component in modern healthcare systems, offers a multitude of functionalities and benefits for seamless data exchange and interoperability. Here are ten core features that highlight its significance:
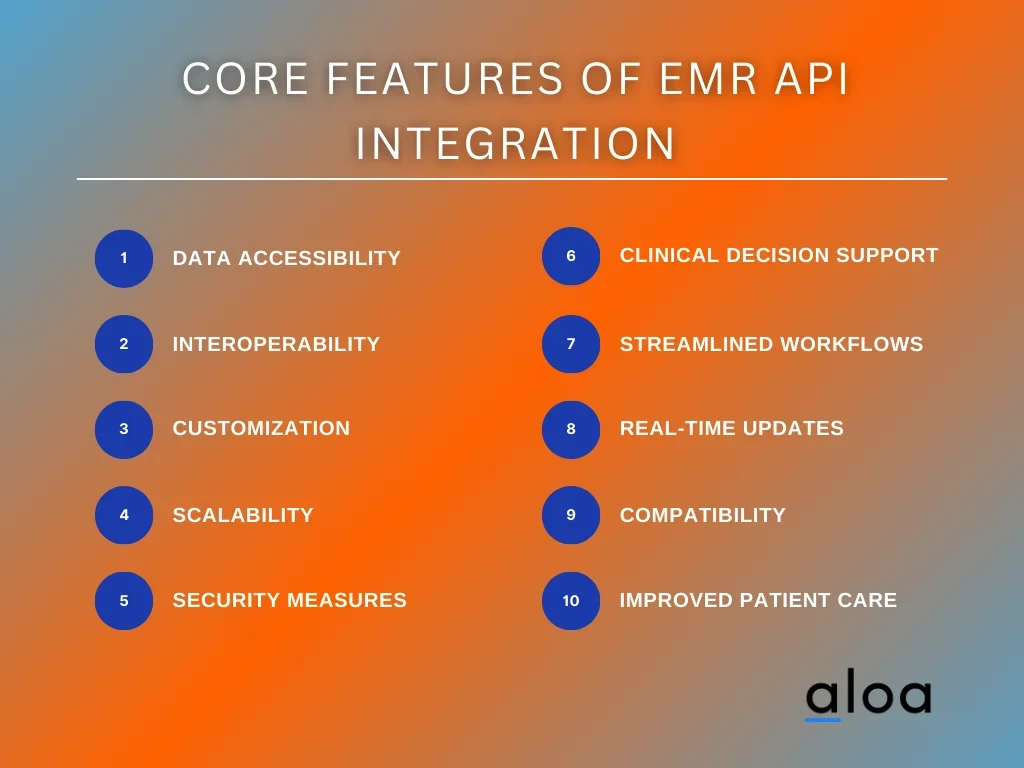
- Data Accessibility: EMR API integration facilitates easy access to Electronic Medical Records (EMRs) and other healthcare data from diverse sources. It ensures real-time access to patient information, promoting timely decision-making.
- Interoperability: It enables interoperability between various healthcare systems, allowing EMRs to communicate and share data securely across different platforms and applications.
- Customization: EMR APIs often offer customizable solutions that cater to the specific needs of healthcare providers, allowing for tailored integrations based on the organization's requirements.
- Scalability: These integrations are designed to scale efficiently, accommodating the growing data needs of healthcare facilities and adapting to evolving technology landscapes.
- Security Measures: Robust security protocols are a hallmark of EMR integration with API, ensuring compliance with stringent healthcare data protection regulations like HIPAA. Encryption, authentication, and authorization mechanisms safeguard patient information.
- Clinical Decision Support: Some EMR APIs offer clinical decision support tools, aiding healthcare professionals in making informed decisions by providing insights and alerts based on patient data.
- Streamlined Workflows: Integration streamlines workflows by reducing manual data entry and automating processes, enabling healthcare providers to focus more on patient care.
- Real-time Updates: EMR integration with API integrations provides real-time updates to EMRs, ensuring that healthcare providers can access the most current patient information during consultations and treatments.
- Compatibility: These integrations are designed to be compatible with a wide range of EMR systems, fostering seamless connectivity and seamless data exchange between disparate systems.
- Improved Patient Care: Ultimately, the primary goal of EMR API integration is to enhance patient care by enabling healthcare professionals to swiftly access comprehensive and updated patient data, leading to better-informed decisions and improved outcomes.
EMR API integration is a pivotal tool in modernizing healthcare systems, fostering efficiency, data-driven decision-making, and, ultimately, superior patient care.
Best Practices for EMR API Integration
In healthcare technology, the seamless integration of Electronic Medical Records (EMR) systems through Application Programming Interfaces (APIs) has become pivotal for efficient and interconnected healthcare delivery. EMR API integration ensures that healthcare providers can access, share, and update patient information across various platforms, leading to improved patient care and streamlined workflows.

Secure Authentication Protocols
Robust authentication protocols are imperative to safeguard patient data during EMR API integration. Utilizing industry-standard methods such as OAuth ensures that only authorized entities can access sensitive health information. This enhances security and aligns with regulatory compliance standards, fostering trust among patients and healthcare providers.
Data Standardization and Interoperability
A key challenge in healthcare integration is the diversity of data formats among different EMR systems. Implementing standardized data formats and fostering interoperability ensure that information flows seamlessly between systems. HL7 and FHIR standards are crucial in standardizing health data, facilitating smoother integration, and reducing the risk of data discrepancies.
Real-Time Data Synchronization
For an effective EMR API integration, real-time data synchronization is paramount. Healthcare professionals require up-to-the-minute information to make informed decisions. APIs that support real-time data updates enable instant access to critical patient data, improving the quality of care and treatment outcomes.
Scalability and Flexibility
The healthcare landscape is dynamic, with changing requirements and evolving technologies. EMR API integrations should be scaled and flexible to accommodate future growth and advancements. Scalable solutions ensure that the integration remains effective as healthcare systems expand or undergo technological upgrades.
Comprehensive Error Handling and Logging
Despite meticulous planning, errors can occur during EMR API integration. Implementing comprehensive error-handling mechanisms and detailed logging systems is essential for diagnosing issues promptly. This proactive approach minimizes downtime, enhances system reliability, and facilitates quicker issue resolution.
Key Takeaway
Recognizing the pivotal role of EMR API integration is imperative for fostering operational excellence. The seamless exchange of patient records, clinical data, and medical information hinges on a strategically streamlined development process. Aloa stands ready to guide businesses and startups through the intricacies of this critical integration. By embracing the power of this integration, healthcare entities can optimize patient care, enhance interoperability, and navigate regulatory compliance with finesse.
For a comprehensive understanding of this transformative process, delve into our resources at resources@aloa.co, where expertise converges with innovation to propel healthcare systems toward a future of efficient and interconnected operations. Elevate your healthcare practices by harnessing the crucial role that EMR API integration plays in shaping the landscape of modern healthcare.

